Analysis of risk factors for cervical lymph node metastasis in middle and lower esophageal squamous cell carcinoma and construction of a diagnostic model
-
摘要:
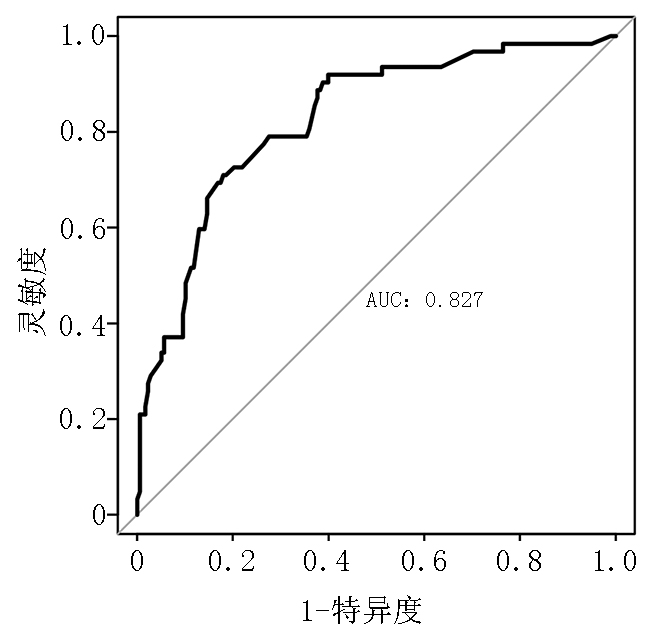
目的 探讨食管中下段鳞癌颈部淋巴结转移的危险因素并构建诊断模型,为临床选择合理手术方式提供参考。 方法 选取2015年1月至2020年6月于河北医科大学第四医院行食管癌根治术+三野淋巴结清扫的240例食管中下段鳞癌患者作为观察对象,依据术后病理分为颈部淋巴结转移组和颈部淋巴结无转移组。采用多因素Logistic 回归分析颈部淋巴结转移的独立危险因素,并建立诊断模型,应用受试者工作特征(ROC)曲线评估其诊断效能。 结果 240例食管中下段鳞癌患者中有62例(25.8%)发生颈部淋巴结转移。Logistic回归分析结果显示,肿瘤最大径、食管旁淋巴结转移、喉返神经旁淋巴结转移和CT诊断颈部淋巴结转移是食管中下段鳞癌颈部淋巴结转移的独立危险因素。诊断模型为P=1/(1+exp(-(-3.764+0.361×肿瘤最大径+1.281×食管旁淋巴结转移+1.614×喉返神经旁淋巴结转移+1.155×CT诊断颈部淋巴结转移))),其阴性预测值为89.89%,阳性预测值为45.16%,准确度为78.33%。ROC曲线分析显示,ROC 曲线下的面积为0.827(95%CI :0.767~0.886),约登指数为0.530,灵敏度和特异度分别为70.97%和82.02%。 结论 肿瘤最大径、食管旁淋巴结转移、喉返神经旁淋巴结转移和CT诊断颈部淋巴结转移是食管中下段鳞癌颈部淋巴结转移的独立危险因素,以此为基础建立的诊断模型具有一定的临床运用价值。 Abstract:Objective To investigate the risk factors of cervical lymph node metastasis in middle and lower esophageal squamous cell carcinoma and construct a diagnostic model to provide clinical strategies for the rational selection of surgical methods. Methods A total of 240 patients with middle and lower esophageal squamous cell carcinoma, who underwent radical esophagectomy and three-field lymph node dissection at The Fourth Hospital of Hebei Medical University from January 2015 to June 2020 were selected as the observation subjects. According to the postoperative pathology, the patients were assigned into the cervical lymph node metastasis group and non-cervical lymph node metastasis group. Multivariate Logistic regression was used to analyze the independent risk factors of cervical lymph node metastasis, and receiver operating characteristic (ROC) curve was used to evaluate the diagnostic performance. Results Among 240 patients, 62 (25.8%) had cervical lymph node metastasis. Multivariate Logistic regression analysis revealed that the largest tumor diameter, paraesophageal lymph node status, recurrent laryngeal nerve lymph node status, and cervical lymph node metastasis status diagnosed by computed tomography (CT) were independent risk factors for cervical lymph node metastasis in middle and lower esophageal squamous cell carcinoma. The diagnostic model: P=1/(1+exp(-(-3.764+ 0.361× largest tumor diameter+1.281×paraesophageal lymph node status+1.614×recurrent laryngeal nerve lymph node status+1.155×cervical lymph node metastasis status diagnosed by CT))). The negative and positive predictive values were 89.89% and 45.16%, respectively. The area under the ROC curve of the diagnostic model constructed according to the independent risk factors was 0.827 (95%CI: 0.767–0.886), and the Youden index was 0.530, corresponding to a sensitivity and specificity of 70.97% and 82.02%, respectively. Conclusions The largest tumor diameter, paraesophageal lymph node status, recurrent laryngeal nerve lymph node status, and cervical lymph node metastasis status diagnosed by CT are independent risk factors for cervical lymph node metastasis of middle and lower esophageal squamous cell carcinoma. The diagnostic model established on this basis has a certain clinical application value. -
表 1 两组患者的临床资料比较
n(%) 临床特征 颈部淋巴结无转移组(n=178) 颈部淋巴结转移组(n=62) χ2/t P 性别 1.498* 0.280 男 114(64.0) 45(72.6) 女 64(36.0) 17(27.4) 年龄(岁) 61.7±6.8 60.3±6.2 1.365** 0.091 肿瘤位置 0.892* 0.390 中段 133(74.7) 50(80.6) 下段 45(25.3) 12(19.4) 肿瘤最大径(cm) 3.3±1.5 4.3±1.8 −4.155** <0.001 肿瘤分化程度 2.989* 0.220 高分化 30(16.8) 5(8.1) 中分化 100(56.2) 37(59.7) 低分化 48(27.0) 20(32.2) T分期(期) 22.984* <0.001 pT1 56(31.5) 4(6.4) pT2 33(18.5) 7(11.3) pT3 74(41.6) 38(61.3) pT4 15(8.4) 13(21.0) 脉管瘤栓 9.662* 0.005 有 14(7.9) 14(22.6) 无 164(92.1) 48(77.4) 神经受侵 3.876* 0.070 有 24(13.5) 15(24.2) 无 154(86.5) 47(75.8) 食管旁淋巴结转移 25.537* <0.001 有 20(11.2) 25(40.3) 无 158(88.8) 37(59.7) 纵隔淋巴结转移 30.985* <0.001 有 15(8.4) 24(38.7) 无 163(91.6) 38(61.3) 腹部淋巴结转移 6.811* 0.011 有 46(25.8) 27(43.5) 无 132(74.2) 35(56.5) 喉返神经旁淋巴结转移 35.389* <0.001 有 41(23.0) 40(64.5) 无 137(77.0) 22(35.5) CT诊断颈部淋巴结转移 13.488* <0.001 有 31(17.4) 25(40.3) 无 147(82.6) 37(59.7) 切除方式 1.690* 0.240 R0 173(97.2) 58(93.5) R1 5(2.8) 4(6.5) *:χ2检验;**:t检验 表 2 颈部淋巴结转移的多因素Logistic回归分析
因素 β OR 95%CI P 肿瘤最大径 0.301 1.351 1.061~1.721 0.015 T分期 0.288 1.334 0.848~2.100 0.213 脉管瘤栓 0.289 1.336 0.483~3.700 0.577 食管旁淋巴结转移 1.082 2.950 1.271~6.844 0.012 纵隔旁淋巴结转移 0.907 2.476 0.979~6.262 0.056 腹部旁淋巴结转移 −0.165 0.848 0.373~1.926 0.693 喉返神经旁淋巴结转移 1.320 3.745 1.809~7.754 <0.001 CT诊断颈部淋巴结转移 0.972 2.644 1.195~5.852 0.016 常数项 −4.237 − − − 表 3 食管中下段鳞癌颈部淋巴结转移的诊断模型
因素 β OR 95%CI P 肿瘤最大径 0.361 1.435 1.147~1.796 0.002 食管旁淋巴结转移 1.281 3.602 1.654~7.841 0.001 喉返神经旁淋巴结转移 1.614 5.023 2.530~9.970 <0.001 CT诊断颈部淋巴结转移 1.155 3.175 1.491~6.763 0.003 常数项 −3.764 − − − 表 4 诊断模型的评价
n (%) 颈部淋巴结转移实际结果 颈部淋巴结转移预测结果 无 有 无 160 34 有 18 28 -
[1] Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries[J]. CA Cancer J Clin, 2021, 71(3):209-249. doi: 10.3322/caac.21660 [2] Chen W, Li H, Zheng R, et al. An initial screening strategy based on epidemiologic information in esophageal cancer screening: a prospective evaluation in a community-based cancer screening cohort in rural China[J]. Gastrointest Endosc, 2021, 93(1):110-118. doi: 10.1016/j.gie.2020.05.052 [3] Leng XF, Daiko H, Han YT, et al. Optimal preoperative neoadjuvant therapy for resectable locally advanced esophageal squamous cell carcinoma[J]. Ann N Y Acad Sci, 2020, 1482(1):213-224. doi: 10.1111/nyas.14508 [4] Zheng Y, Li Y, Liu X, et al. Minimally invasive versus open McKeown for patients with esophageal cancer: aretrospective study[J]. Ann Surg Oncol, 2021, 28(11):6329-6336. doi: 10.1245/s10434-021-10105-y [5] Ajani JA, D'Amico TA, Bentrem DJ, et al. Esophageal and esophagogastric junction cancers, version 2.2019, NCCN vlinicalpractice guidelines in oncology[J]. J Natl Compr Canc Netw, 2019, 17(7):855-883. doi: 10.6004/jnccn.2019.0033 [6] Borggreve AS, Kingma BF, Domrachev SA, et al. Surgical treatment of esophageal cancer in the era of multimodality management[J]. Ann N Y Acad Sci, 2018, 1434(1):192-209. doi: 10.1111/nyas.13677 [7] Hamai Y, Emi M, Ibuki Y, et al. Distribution of lymph node metastasis in esophageal squamous cell carcinoma after trimodal therapy[J]. Ann Surg Oncol, 2021, 28(3):1798-1807. doi: 10.1245/s10434-020-09106-0 [8] Jung MK, Schmidt T, Chon SH, et al. Current surgical treatment standards for esophageal and esophagogastric junction cancer[J]. Ann N Y Acad Sci, 2020, 1482(1):77-84. doi: 10.1111/nyas.14454 [9] Shi Y, Wang A, Yu S, et al. Thoracoscopic-laparoscopic Ivor-Lewis surgery vs. McKeown surgery in the treatment of thoracic middle-lower segment esophageal cancer[J]. J BUON, 2021, 26(3):1062-1069. [10] Ishibashi N, Maebayashi T, Nishimaki H, et al. Computed tomography of lymph node metastasis before and after radiation therapy: correlations with residual tumour[J]. In Vivo, 2020, 34(5):2721-2725. [11] Li H, Fang W, Yu Z, et al. Chinese expert consensus on mediastinal lymph node dissection in esophagectomy for esophageal cancer (2017 edition)[J]. J Thorac Dis, 2018, 10(4):2481-2489. doi: 10.21037/jtd.2018.03.175 [12] Yang CS, Chen XL. Research on esophageal cancer: with personal perspectives from studies in China and Kenya[J]. Int J Cancer, 2021, 149(2):264-276. doi: 10.1002/ijc.33421 [13] Ozawa S. Minimally invasive surgery for esophageal cancer in Japan[J]. Ann Thorac Cardiovasc Surg, 2020, 26(4):179-183. doi: 10.5761/atcs.ed.20-00079 [14] Hollis AC, Quinn LM, Hodson J, et al. Prognostic significance of tumor length in patients receiving esophagectomy for esophageal cancer[J]. J Surg Oncol, 2017, 116(8):1114-1122. doi: 10.1002/jso.24789 [15] Haisley KR, Hart KD, Fischer LE, et al. Increasing tumor length is associated with regional lymph node metastases and decreased survival in esophageal cancer[J]. Am J Surg, 2016, 211(5):860-866. doi: 10.1016/j.amjsurg.2016.01.007 [16] Liebermann-Meffert D. Anatomical basis for the approach and extent of surgical treatment of esophageal cancer[J]. Dis Esophagus, 2001, 14(2):81-84. doi: 10.1046/j.1442-2050.2001.00160.x [17] Wang A, Lu L, Fan J, et al. Lymph node metastatic patterns and its clinical significance for thoracic superficial esophageal squamous cell carcinoma[J]. J Cardiothorac Surg, 2020, 15(1):262. doi: 10.1186/s13019-020-01302-z [18] Liu Y, Zou ZQ, Xiao J, et al. A nomogram prediction model for recurrent laryngeal nerve lymph node metastasis in thoracic oesophageal squamous cell carcinoma[J]. J Thorac Dis, 2019, 11(7):2868-2877. [19] Wu J, Chen QX, Zhou XM, et al. Does recurrent laryngeal nerve lymph node metastasis really affect the prognosis in node-positive patients with squamous cell carcinoma of the middle thoracic esophagus[J]? BMC Surg, 2014, 14:43. [20] Chen C, Ma Z, Shang X, et al. Risk factors for lymph node metastasis of the left recurrent laryngeal nerve in patients with esophageal squamous cell carcinoma[J]. Ann Transl Med, 2021, 9(6):476. doi: 10.21037/atm-21-377 [21] Li H, Yang S, Zhang Y, et al. Thoracic recurrent laryngeal lymph node metastases predict cervical node metastases and benefit from three-field dissection in selected patients with thoracic esophageal squamous cell carcinoma[J]. J Surg Oncol, 2012, 105(6):548-552. [22] Lee HN, Kim JI, Shin SY, et al. Combined CT texture analysis and nodal axial ratio for detection of nodal metastasis in esophageal cancer[J]. Br J Radiol, 2020, 93(1111):20190827. doi: 10.1259/bjr.20190827 [23] Su GY, Xu XQ, Zhou Y, et al. Texture analysis of dual-phase contrast-enhanced CT in the diagnosis of cervical lymph node metastasis in patients with papillary thyroid cancer[J]. Acta Radiol, 2021, 62(7):890-896. -



 下载:
下载:


