Research progress on the association between calcium–gene interactions and the risk of colorectal adenoma
-
摘要: 结直肠癌是胃肠道中常见的恶性肿瘤,近几年,结直肠癌的发病率和死亡率保持着上升趋势,居高不下。而结直肠腺瘤是结直肠癌最重要的癌前病变,其发病机制对于结直肠癌早期诊疗至关重要。结直肠腺瘤的发病机制较为复杂,一般涉及多个基因的相互作用和信号通路。且钙剂与结直肠腺瘤的关联研究在近年来也引起广泛关注。因此,本文对钙与基因的相互作用和结直肠腺瘤发病风险的关系进行综述,为结直肠癌的早期筛查、诊断和早期治疗提供参考。Abstract: Colorectal cancer is a common malignancy in gastrointestinal tract. In recent years, the incidence and mortality rates of colorectal cancer have maintained an upward trend and remain high. Colorectal adenoma is the most prominent precancerous lesion associated with colorectal cancer, and its pathogenesis is very important for the early diagnosis and treatment of colorectal cancer. The pathogenesis of colorectal adenoma is complicated, generally involving interactions among multiple genes and signaling pathways. Studies of associations between calcium and colorectal adenoma have attracted widespread attention in recent years. This review summarizes the relationships between calcium and gene interactions and the risk of colorectal adenoma, providing references for the early screening, diagnosis, and early treatment of colorectal cancer.
-
Key words:
- colorectal adenoma /
- gene /
- calcium /
- chemoprevention
-
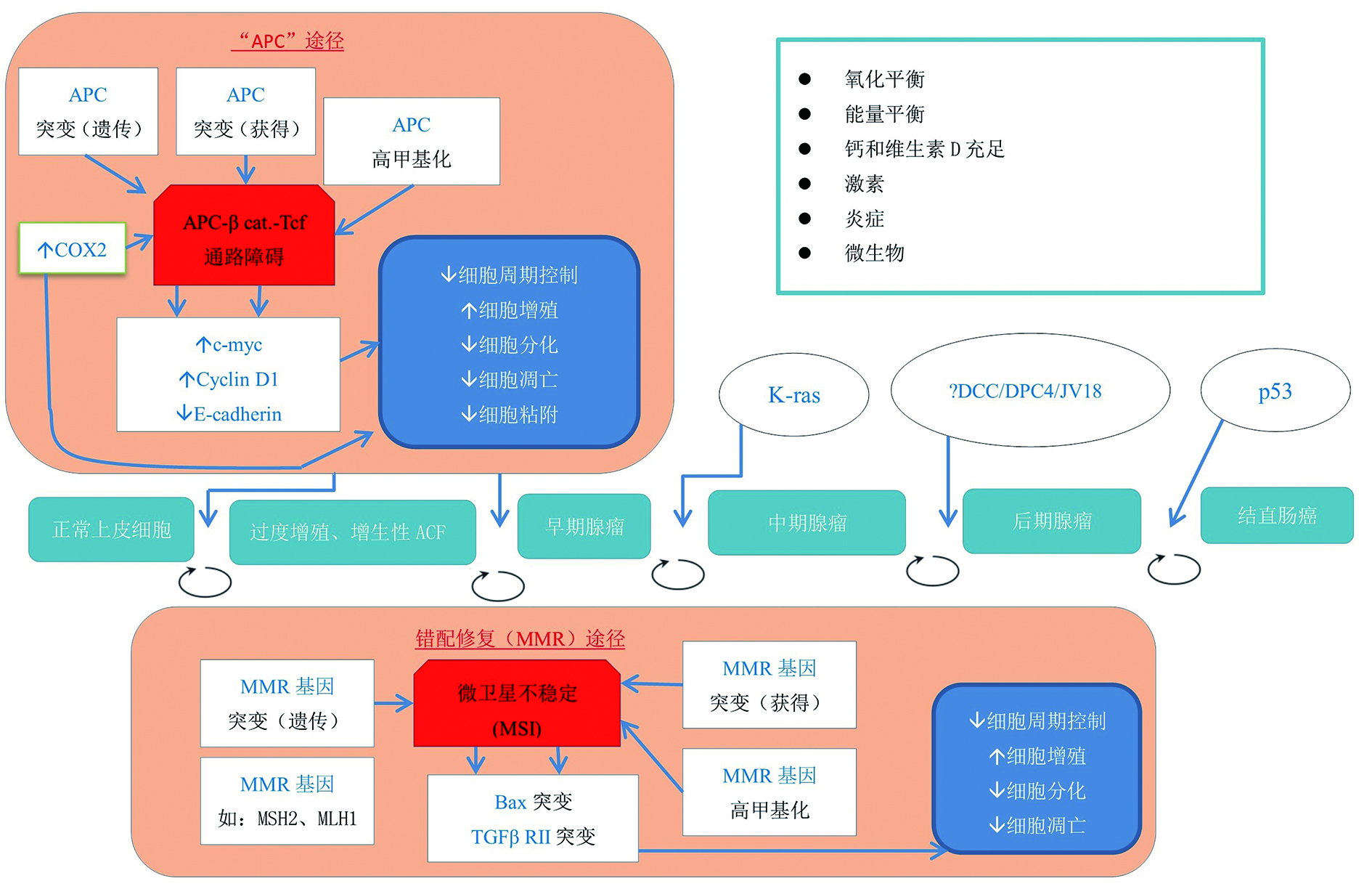
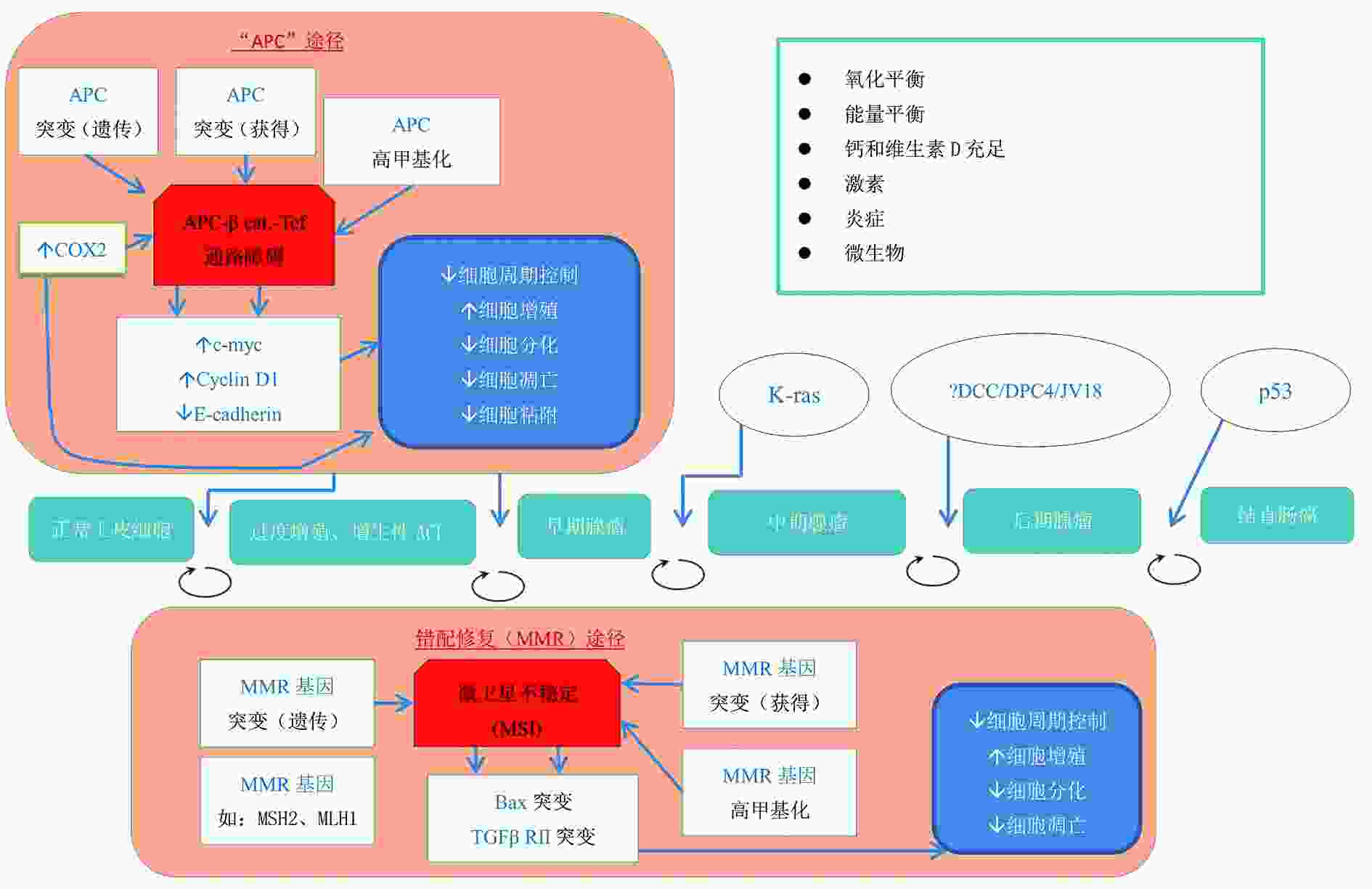
图 1 结直肠癌发生分子基础[15]
表 1 结直肠肿瘤风险的分子表型生物标志物[15]
序号 种类 生物标志物表达 1 结肠癌发生途径 APC途径 APC, E-cadherin MMR途径 MSH2、MLH1、TGFβ RⅡ、bax 2 细胞周期 细胞增殖 短期 Mib-1(Ki-67) 长期 hTERT 细胞分化 p21 细胞凋亡 抑制 bcl-2 促进 bax 3 细胞黏附 E-cadherin 4 炎症 COX-2、CRP、 IL-6、 IL-1β、 IL-8、 IL-10、 TNFα 5 氧化平衡 8-OH-dG 6 维生素D/钙代谢 CaSR、VDR、 CYP27B1、CYP24 7 生长因子信号 TGFα、 TGFβ1、 IGF-Ⅰ、 IGFBP3 -
[1] Sung H, Ferlay J, Siegel RL. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin., 2021, 71(3):209-249. doi: 10.3322/caac.21660 [2] Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2021[J]. CA Cancer J Clin, 2021, 71(1):7-33. doi: 10.3322/caac.21654 [3] Bailey RL, Akabas SR, Paxson EE, et al. Total usual intake of shortfall nutrients varies with poverty among US adults[J]. J Nutr Educ Behav. 2017, 49(8): 639-646. [4] Saito T, Chambers JK, Nakashima K, et al. Histopathologic features of colorectal adenoma and adenocarcinoma developing within inflammatory polyps in miniature dachshunds[J]. Vet Pathol, 2018, 55(5):654-662. doi: 10.1177/0300985818777798 [5] Baron JA, Beach M, Mandel JS, et al. Calcium supplements for the prevention of colorectal adenomas. Calcium polyp prevention study group[J]. N Engl J Med, 1999, 340(2):101-107. doi: 10.1056/NEJM199901143400204 [6] Sun P, Zhu X, Shrubsole MJ, et al. Genetic variation in SLC7A2 interacts with calcium and magnesium intakes in modulating the risk of colorectal polyps[J]. J Nutr Biochem, 2017, 47:35-40. doi: 10.1016/j.jnutbio.2017.04.016 [7] Emami MH, Salehi M, Hassanzadeh Keshteli A, et al. Calcium and dairy products in the chemoprevention of colorectal adenomas: a systematic review and meta-analysis[J]. Crit Rev Food Sci Nutr, 2021,(61):1-25. [8] Wang Y, Wactawski-Wende J, Sucheston-Campbell LE, et al. The influence of genetic susceptibility and calcium plus vitamin D supplementation on fracture risk[J]. Am J Clin Nutr, 2017, 105(4):970-979. doi: 10.3945/ajcn.116.144550 [9] Brink M, Weijenberg MP, de Goeij AF. P. M, et al. Fat and K-ras mutations in sporadic colorectal cancer in The Netherlands Cohort Study[J]. Carcinogenesis, 2004, 25(9):1619-1628. doi: 10.1093/carcin/bgh177 [10] Schulz MD, Atay C, Heringer J, et al. High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity[J]. Nature, 2014, 514(7523):508-512. [11] Mehta M, Shike M. Diet and physical activity in the prevention of colorectal cancer[J]. J Natl Compr Canc Netw, 2014, 12(12):1721-1726. doi: 10.6004/jnccn.2014.0174 [12] Lipkin M. Early development of cancer chemoprevention clinical trials: studies of dietary calcium as a chemopreventive agent for human subjects[J]. Eur J Cancer Prev, 2002, 11(2):S65-S70. [13] Um CY, Fedirko V, Flanders WD, et al. Associations of calcium and milk product intakes with incident, sporadic colorectal adenomas[J]. Nutr Cancer, 2017, 69(3):416-427. [14] Huang D, Lei S, Wu Y, et al. Additively protective effects of vitamin D and calcium against colorectal adenoma incidence, malignant transformation and progression: A systematic review and meta-analysis[J]. Clin Nutr, 2020, 39(8):2525-2538. doi: 10.1016/j.clnu.2019.11.012 [15] Bostick RM. Effects of supplemental vitamin D and calcium on normal colon tissue and circulating biomarkers of risk for colorectal neoplasms[J]. J Steroid Biochem Mol Biol, 2015, 148:86-95. doi: 10.1016/j.jsbmb.2015.01.010 [16] Eshghifar N, Farrokhi N, Naji T, et al. Tumor suppressor genes in familial adenomatous polyposis[J]. Gastroenterol Hepatol Bed Bench, 2017, 10(1):3-13. [17] Ahearn TU, Shaukat A, Flanders WD, et al. Markers of the APC/beta-catenin signaling pathway as potential treatable, preneoplastic biomarkers of risk for colorectal neoplasms[J]. Cancer Epidemiol Biomarkers Prev, 2012, 21(6):969-979. doi: 10.1158/1055-9965.EPI-12-0126 [18] Liu S, Barry EL, Baron JA, et al. Effects of supplemental calcium and vitamin D on the APC/β‐catenin pathway in the normal colorectal mucosa of colorectal adenoma patients[J]. Mol Carcinog, 2017, 56(2):412-424. doi: 10.1002/mc.22504 [19] Rubenstein JH, Enns R , Heidelbaugh J, et al. American gastroenterological association institute guideline on the diagnosis and management of Lynch syndrome[J]. Gastroenterology, 2015, 149(3):777-782. [20] Sidelnikov E, Bostick RM, Flanders WD, et al. Colorectal mucosal expression of MSH2 as a po-tential biomarker of risk for colorectal neoplasms[J]. Cancer Epidemiol Biomarkers Prev, 2009, 18(11):2965-2973. [21] Sidelnikov E, Bostick RM, Flanders WD, et al. MutL-homolog 1 expression and risk of incident, sporadic colorectal adenoma: Search for prospective biomarkers of risk for colorectal cancer[J]. Cancer Epidemiol Biomarkers Prev, 2009, 18(5):1599-1609. doi: 10.1158/1055-9965.EPI-08-0800 [22] Sidelnikov E, Bostick RM, Dana FW, et al. Effects of calcium and vitamin D on MLH1 and MSH2 expression in rectal mucosa of sporadic colorectal adenoma patients[J]. Cancer Epidemiol Biomarkers Prev, 2010, 19(4):1022-1032. doi: 10.1158/1055-9965.EPI-09-0526 [23] Kwan AK, Um CY, Rutherford RE, et al. Effects of vitamin D and calcium on expression of MSH2 and transforming growth factors in normal-appearing colorectal mucosa of sporadic colorectal adenoma patients: A randomized clinical trial[J]. Mol Carcinog, 2019, 58(4):511-523. doi: 10.1002/mc.22945 [24] Tu H, Ahearn TU, Danie CR, et al. Transforming growth factors and receptor as potential modif-iable pre-neoplastic biomarkers of risk for colorectal neoplasms[J]. Mol Carcinog, 2015, 54(9):821-830. doi: 10.1002/mc.22152 [25] Tu H, Flanders WD, Ahearn TU, et al. Effects of calcium and vitamin D3 on transforming growth factors in rectal mucosa of sporadic colorectal adenoma patients: A randomized controlled trial[J]. Mol Carcinog, 2015, 54(4):270-280. doi: 10.1002/mc.22096 [26] Davenpor JR, Cai Q, Ness RM, et al. Evaluation of pro-inflammatory markers plasma C-reactiveprotein and urinary prostaglandin-E2 metabolite in colorectal adenoma risk[J]. Mol Carcinog, 2016, 55(8):1251-1261. doi: 10.1002/mc.22367 [27] Hull MA, Cuthbert RJ, Ko CWS, et al. Paracrine cyclooxygenase-2 activity by macrophages drives colorectal adenoma progression in the Apc Min/+ mouse model of intestinal tumorigenesis[J]. Sci Rep, 2017, 7(1):6074. doi: 10.1038/s41598-017-06253-5 [28] Gibbs DC, Fedirko V, Baron JA, et al. Inflammation modulation by vitamin D and calcium in the morphologically normal colorectal mucosa of patients with colorectal adenoma in a clinical trial[J]. Cancer Prev Res (Phila)., 2021, 14(1):65-76. [29] Suren D, Yildirim M, Kaya V, et al. Loss of tight junction proteins (Claudin 1, 4, and 7) correlates with aggressive behavior in colorectal carcinoma[J]. Med Sci MonitMedical Science Monitor, 2014, 20:1255-1262. [30] Coleman O, Haller D. Microbe-mucus interface in the pathogenesis of colorectal cancer[J]. Cancers (Basel), 2021, 13(4):616. doi: 10.3390/cancers13040616 [31] Yin Z, Pintea V, Lin Y, et al. Vitamin D enhances corneal epithelial barrier function[J]. Invest Ophthalmol Vis Sci, 2011, 52(10):7359-7364. [32] Mandle HB, Jahan FA, Bostick RM, et al. Effects of supplemental calcium and vitamin D on tight-junction proteins and mucin-12 expression in the normal rectal mucosa of colorectal adenoma patients[J]. Mol Carcinog, 2019, 58(7):1279-1290. [33] Zhu X, Liang J, Shrubsole MJ, et al. Calcium intake and ion transporter genetic polymorphisms interact in human colorectal neoplasia risk in a 2-Phase Study[J]. J Nutr, 2014, 144(11):1734-1741. doi: 10.3945/jn.114.196709 [34] Zhao J, Zhu X, Shrubsole MJ, et al. Interactions between calcium intake and polymorphisms in genes essential for calcium reabsorption and risk of colorectal neoplasia in a two-phase study[J]. Mol Carcinog, 2017, 56(10):2258-2266. doi: 10.1002/mc.22678 [35] Su F, Wang B-F, Zhang T, et al. TRPM7 deficiency suppresses cell proliferation, migration, and invasion in human colorectal cancer via regulation of epithelial-mesenchymal transition[J]. Cancer Biomark., 2019, 26(4):451-460. doi: 10.3233/CBM-190666 [36] Gerda E Breitwieser. Pharmacoperones and the calcium sensing receptor: Exogenous and endogenous regulators[J]. Pharmacol Res, 2014:30-37. [37] Abhishek A, Prinz-Wohlgenannt M, Tennakoon S, et al. The calciumsensing receptor: A promising target for prevention of colorectal cancer[J]. Biochim Biophys Acta, 2015, 1853(9):2158-2167. [38] Zhu X, Shrubsole MJ, Ness RM, et al. Calcium/magnesium intake ratio, but not magnesium intake, interacts with genetic polymorphism in relation to colorectal neoplasia in a two-phase study[J]. Mol Carcinog , 2016, 55(10):1449-1457. -



 下载:
下载: