-
摘要:
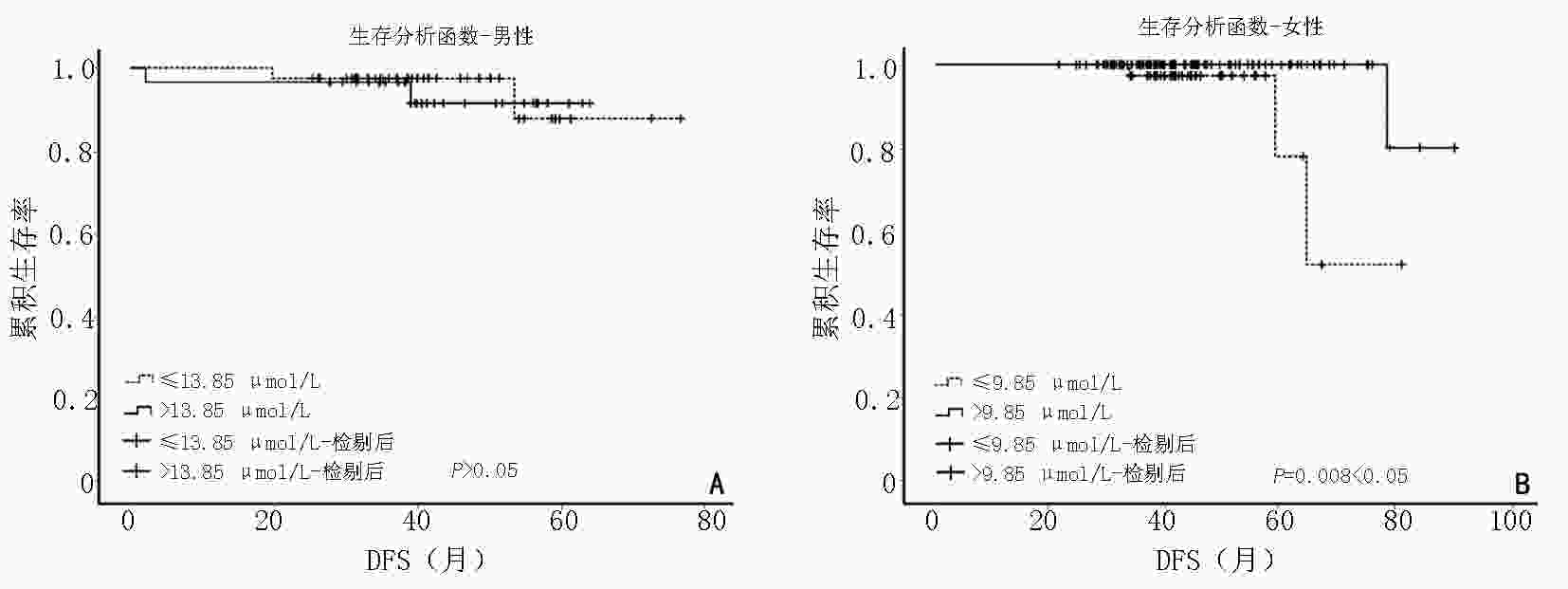
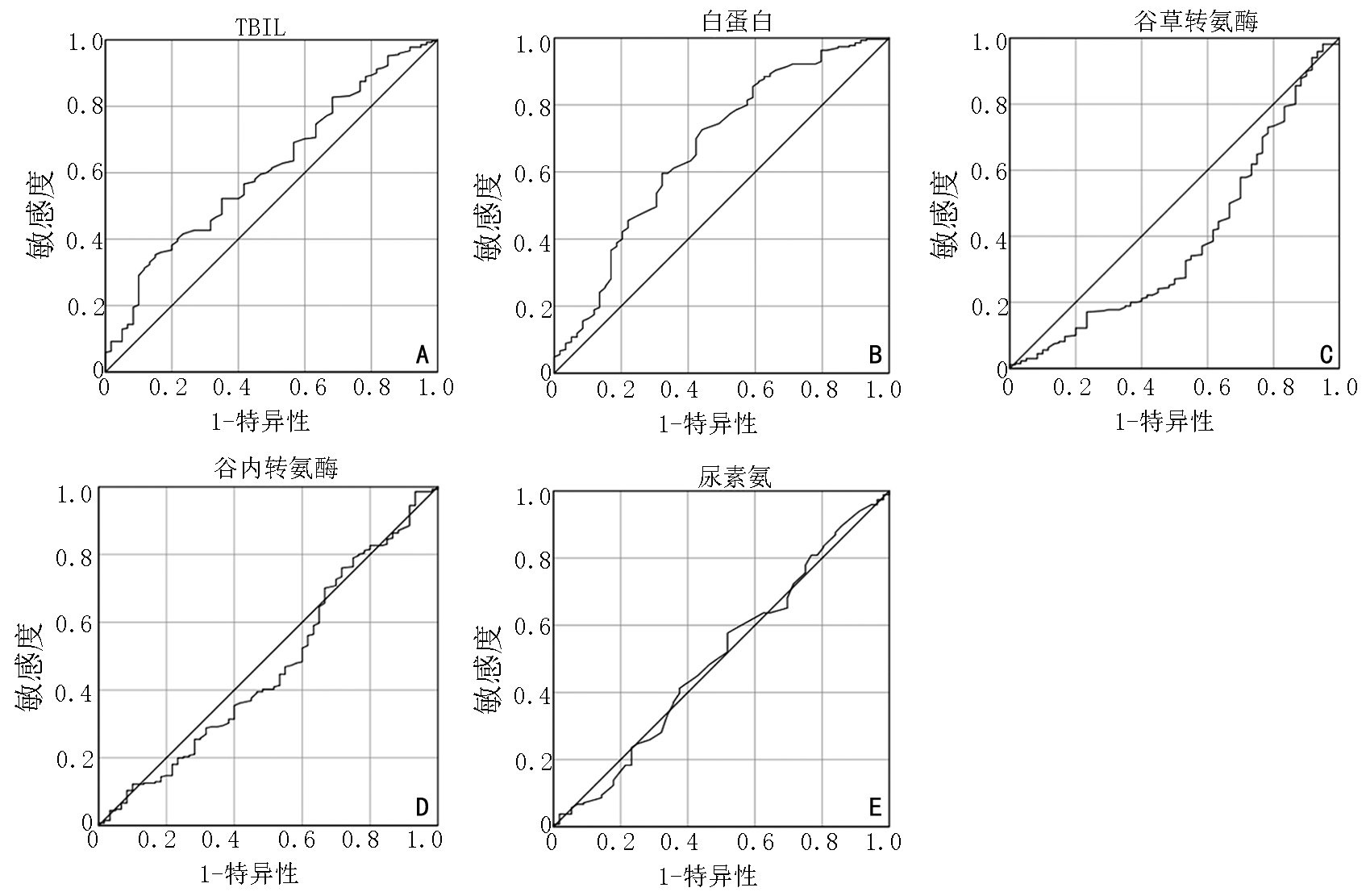
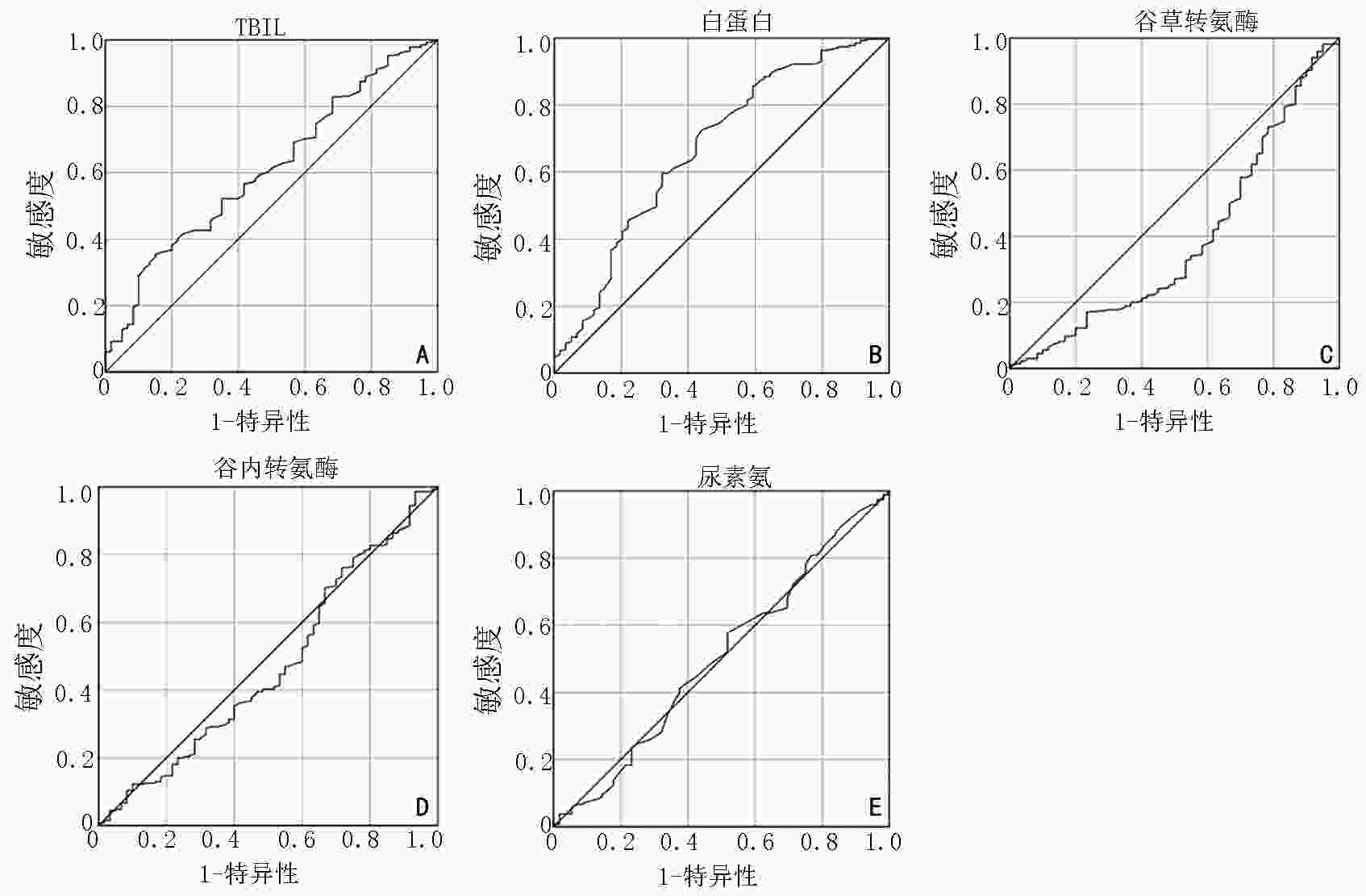
目的 研究血清总胆红素(total bilirubin,TBIL)与非小细胞肺癌(non-small cell lung cancer,NSCLC)患者临床病理特征以及炎症细胞之间的关系,探讨血清TBIL对NSCLC患者治疗的指导意义以及预后价值。 方法 回顾性分析2017年3月至2020年12月于上海中医药大学附属市中医医院就诊的NSCLC患者332例,收集患者临床资料,并通过电话、门诊复诊等方式进行随访,采用Logistic回归分析进行单因素分析,采用Kaplan-Meier生存曲线进行生存分析。 结果 NSCLC患者血清TBIL水平在不同性别中存在差异,男性高于女性(P<0.05),但在不同年龄、有无吸烟史及患病时间中无显著性差异(P>0.05);在不同淋巴浸润程度、是否存在远处转移和不同肿瘤分期中,血清TBIL表达存在显著性差异(P<0.05)。Logistic回归分析发现TBIL、白蛋白、谷草转氨酶水平与患者预后具有显著相关性(P<0.05);当女性患者TBIL>9.85 μmol/L时,患者无病生存期相比TBIL≤9.85 μmol/L时延长,男性患者TBIL水平与无病生存期无明显相关性(P>0.05)。根据TBIL水平将患者分为高水平和低水平组,男性患者淋巴细胞比例在TBIL高水平组较高,中性粒细胞淋巴细胞比值(neutrophil- lymphocyte ratio,NLR)在高水平组较低;女性患者淋巴细胞比例在高水平组较高,NLR、CD3、CD4细胞比例在高水平组较低(P<0.05)。 结论 血清TBIL在NSCLC早期患者中的表达水平高于进展期患者,有望成为NSCLC的治疗指导依据;TBIL与中性粒细胞和NLR之间可能存在协同作用,共同在肺癌免疫调节中发挥抗肿瘤作用。 Abstract:Objective To investigate the relationship between serum total bilirubin (TBIL) and the clinicopathological characteristics and inflammatory cells of non-small cell lung cancer (NSCLC) patients, and to explore the significance of serum TBIL in guiding the treatment of NSCLC patients and its prognostic value. Methods A retrospective analysis of 332 patients with NSCLC who attended Municipal Hospital of Traditional Chinese Medicine Affiliated to Shanghai University of Traditional Chinese Medicine from March 2017 to December 2020, with clinical data collected and followed up by telephone and outpatient follow-up, was performed using Logistic regression analysis for univariate analysis and Kaplan-Meier survival curve for survival analysis. Results The serum TBIL levels of NSCLC patients differed in genders, with males being higher than females (P<0.05), but there were no significant differences among ages, smoking and the duration of disease (P>0.05); in addition, serum TBIL was differentially expressed by degree of lymphatic infiltration, whether or not distant metastasis was present, and TNM stage (P<0.05). Logistic regression analysis showed that TBIL, albumin and glutamate aminotransferase levels had a significant effect on prognosis of the disease (P<0.05); female patients had a better prognosis when their TBIL levels were greater than 9.85 μmol/L when compared with those with TBIL ≤9.85 μmol/L, but there was no correlation between TBIL levels and disease-free survival in male patients (P>0.05). Patients were assigned into high or low level groups according to TBIL levels. The percentage of lymphocytes in male patients was highly expressed in the high level group and neutrophil-lymphocyte ratio (NLR) values were low in the high level group; The percentage of lymphocytes in female patients was highly expressed in the high level group, but the NLR values and CD3, CD4 cell proportions were low in the high level group (P<0.05). Conclusions The expression level of serum TBIL was higher in NSCLC patients with early-stage than in patients with progressive stage, which is expected to be a basis for guiding the treatment of NSCLC; there may be synergistic effect between TBIL and neutrophils and NLR, which together play an anti-tumor role in immune regulation of lung cancer. -
Key words:
- non-small cell lung cancer (NSCLC) /
- bilirubin /
- oxidative stress /
- tumor immunity
-
表 1 血清总胆红素水平与肺癌临床病例特征的关系
项目 n(%) 血清TBIL(μmol/L) Z P 性别 −2.375 0.018 男 133(40.1) 13.1(10.9,15.5) 女 199(59.9) 12.3(10.1,14.8) 年龄(岁) −1.273 0.203 ≤63 173(52.1) 12.4(10.1,15) >63 159(47.9) 12.8(10.95,14.8) 吸烟史 −1.472 0.141 有 77(76.8) 13.2(10.8,15) 无 255(23.2) 12.4(10.25,14.9) 肿瘤直径(cm) −0.440 0.660 ≤2 200(60.2) 12.7(10.4,15.5) >2 101(30.4) 12.6(10.4,14.5) 未知 31(9.4) 12.1(9.6,15.0) 淋巴结浸润 −2.357 0.018 无 268(80.7) 12.8(10.45,15.5) 有 64(19.3) 11.8(9.35,13.75) 远处转移 −2.053 0.040 无 290(87.3) 12.75(10.4,15.5) 有 42(12.7) 11.6(8.9,13.7) 分期 −2.779 0.005 Ⅰ~Ⅱ期 272(81.9) 13.77±0.32 Ⅲ~Ⅳ期 60(18.1) 11.66±0.50 患病时间(年) −1.387 0.165 ≤2 206(62.0) 12.3(10,15) >2 126(38.0) 12.9(11,14.8) 表 2 二元Logitic回归分析肿瘤分期病情程度的影响因素
项目 B P OR 95%置信区间 性别 −0.662 0.125 0.516 0.222~1.201 年龄 0.026 0.212 1.026 0.985~1.068 患病时间(年) <0.010 0.822 1.000 1.000~1.000 TBIL −0.127 0.012 0.881 0.798~0.973 总蛋白 0.004 0.078 1.004 1.000~1.000 白蛋白 −0.241 <0.010 0.786 0.687~0.899 球蛋白 0.020 0.563 1.029 0.933~1.135 谷草转氨酶 0.091 0.004 1.095 1.029~1.165 谷丙转氨酶 −0.047 0.027 0.954 0.915~0.995 γ−谷氨酰转肽酶 0.003 0.730 1.003 0.984~1.023 前白蛋白 0.001 0.717 1.001 0.995~1.007 总胆固醇 −0.229 0.233 0.798 0.545~1.159 甘油三酯 0.193 0.257 1.213 0.869~1.694 尿素氮 −0.411 0.024 0.663 0.464~0.947 血肌酐 0.026 0.052 1.027 1.000~1.055 尿酸 0.002 0.083 1.002 1.000~1.005 表 3 男性患者不同TBIL水平炎症细胞表达情况
男性 低水平组 高水平组 Z/F P WBC 7.36(3.13,74.50) 6.00(3.05,12.43) −1.16 0.25 中性粒细胞(%) 58.76±1.35 57.17±1.65 2.03 0.16 淋巴细胞(%) 27.85(2.84,74.70) 31.60(8.40,55.80) −2.58 0.01 NLR 2.35(0.54,20.71) 1.76(0.55,8.67) −3.19 <0.01 CD3(%) 60.83±1.48 63.93±1.88 1.62 0.21 CD4(%) 33.31±1.06 34.46±1.45 0.78 0.38 CD8(%) 22.76(7.52,44.10) 23.54(10.49,58.83) −0.32 0.75 表 4 女性患者不同TBIL水平炎症细胞表达情况
女性 低水平组 高水平组 Z/F P WBC 5.98(3.65,10.27) 5.77(1.17,9.80) −0.57 0.57 中性粒细胞(%) 57.40±1.66 56.70±0.72 0.56 0.46 淋巴细胞(%) 30.03±1.59 32.85±0.71 2.73 0.10 NLR 1.93(0.79,6.58) 1.64(0.65,8.24) −2.20 0.03 CD3(%) 69.69(22.98,79.52) 64.91(40.36,85.81) −2.53 0.01 CD4(%) 38.06±1.40 35.14±0.65 1.37 0.04 CD8(%) 24.76±1.38 23.66±0.67 1.98 0.16 -
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020[J]. CA Cancer J Clin, 2020, 70(1):7-30. doi: 10.3322/caac.21590 [2] 吴晋楠.肺癌肿瘤微环境中白细胞介素的研究进展[J].临床肺科杂志,2019,24(12):2280-2283. doi: 10.3969/j.issn.1009-6663.2019.12.034 [3] Sies H. Oxidative stress: a concept in redox biology and medicine[J]. Redox Biol, 2015, 4:180-183. [4] Chikara S, Nagaprashantha LD, Singhal J, et al. Oxidative stress and dietary phytochemicals: Role in cancer chemoprevention and treatment[J]. Cancer Lett, 2018, 413:122-134. doi: 10.1016/j.canlet.2017.11.002 [5] Abouzed TK, Althobaiti F, Omran AF, et al. The chemoprevention of spirulina platensis and garlic against diethylnitrosamine induced liver cancer in rats via amelioration of inflammatory cytokines expression and oxidative stress[J]. Toxicol Res (Camb), 2022, 11(1):22-31. [6] Muhsain SN, Lang MA, Abu-Bakar A. Mitochondrial targeting of bilirubin regulatory enzymes: An adaptive response to oxidative stress[J]. Toxicol Appl Pharmacol, 2015, 282(1):77-89. doi: 10.1016/j.taap.2014.11.010 [7] Sedlak TW, Saleh M, Higginson DS, et al. Bilirubin and glutathione have complementary antioxidant and cytoprotective roles[J]. Proc Natl Acad Sci U S A, 2009, 106(13):5171-5176. doi: 10.1073/pnas.0813132106 [8] Gazzin S, Vitek L, Watchko K, et al. A novel perspective on the biology of bilirubin in health and disease[J]. Trends Mol Med, 2016, 22(9):758-768. doi: 10.1016/j.molmed.2016.07.004 [9] Ollinger R, Kogler P, Troppmair J, et al. Bilirubin inhibits tumor cell growth via activation of ERK[J]. Cell Cycle, 2007, 6(24):3078-3085. doi: 10.4161/cc.6.24.5022 [10] Yueh MF, Bonzo JA, TukeyRH. The role of Ah receptor in induction of human UDP-glucuronosyltransferase 1A1[J]. Methods Enzymol, 2005, 400:75-91. [11] Takeda TA, Mu A, Tai TT, et al. Continuous de novo biosynthesis of haem and its rapid turnover to bilirubin are necessary for cytoprotection against cell damage[J]. Sci Rep, 2015, 5:10488. doi: 10.1038/srep10488 [12] Dietrich C, Kaina B. The aryl hydrocarbon receptor (AhR) in the regulation of cell-cell contact and tumor growth[J]. Carcinogenesis, 2010, 31(8):1319-1328. doi: 10.1093/carcin/bgq028 [13] Zucker SD, Horn PS, Sherman KE. Serum bilirubin levels in the U. S. population: gender effect and inverse correlation with colorectal cancer[J]. Hepatology, 2004, 40(4):827-835. doi: 10.1002/hep.1840400412 [14] Lerner-Marmarosh N, Miralem T, Gibbs PE, et al. Human biliverdin reductase is an ERK activator; hBVR is an ERK nuclear transporter and is required for MAPK signaling[J]. Proc Natl Acad Sci U S A, 2008, 105(19):6870-6875. doi: 10.1073/pnas.0800750105 [15] Kravets A, Hu Z, Miralem T, et al. Biliverdin reductase, a novel regulator for induction of activating transcription factor-2 and heme oxygenase-1[J]. J Biol Chem, 2004, 279(19):19916-19923. doi: 10.1074/jbc.M314251200 [16] Miralem T, Lerner-Marmarosh N, Gibbs PE, et al. The human biliverdin reductase-based peptide fragments and biliverdin regulate protein kinase Cδ activity: the peptides are inhibitors or substrate for the protein kinase C[J]. J Biol Chem, 2012, 287(29):24698-24712. doi: 10.1074/jbc.M111.326504 [17] He MM, Fang Z, Hang D, et al. Circulating liver function markers and colorectal cancer risk: A prospective cohort study in the UK Biobank[J]. Int J Cancer, 2021, 148(8):1867-1878. doi: 10.1002/ijc.33351 [18] Horsfall LJ, Burgess S, Hall I, et al. Genetically raised serum bilirubin levels and lung cancer: a cohort study and Mendelian randomisation using UK Biobank[J]. Thorax, 2020, 75(11):955-964. doi: 10.1136/thoraxjnl-2020-214756 [19] Wei TT, Wang LL, Yin JR, et al. Relationship between red blood cell distribution width, bilirubin, and clinical characteristics of patients with gastric cancer[J]. Int J Lab Hematol, 2017, 39(5):497-501. doi: 10.1111/ijlh.12675 [20] 赵韧,李小虎,程自平,等.血清胆红素水平与冠脉病变的关系[J].安徽医学,2014,35(1):12-15. doi: 10.3969/j.issn.1000-0399.2014.01.004 [21] Xu X, Ai F, Huang M. Deceased serum bilirubin and albumin levels in the assessment of severity and mortality in patients with acute pancreatitis[J]. Int J Med Sci, 2020, 17(17):2685-2695. doi: 10.7150/ijms.49606 [22] Horsfall LJ, Rait G, Walters K, et al. Serum bilirubin and risk of respiratory disease and death[J]. JAMA, 2011, 305(7):691-697. doi: 10.1001/jama.2011.124 [23] 范红星,倪建勋,薄彪,等.术前白蛋白-胆红素评分以及其与CA19-9联合作为胰腺癌患者预后指标的临床价值[J].中国普通外科杂志,2020,29(3):310-316. [24] 左红,王述进,冯佳,等.血清总胆红素、糖化白蛋白、糖化血红蛋白与糖尿病血管并发症的关系[J].中国动脉硬化杂志,2019,27(9):787-790. doi: 10.3969/j.issn.1007-3949.2019.09.011 [25] Seyed Khoei N, Jenab M, Murphy N, et al. Circulating bilirubin levels and risk of colorectal cancer: serological and Mendelian randomization analyses[J]. BMC Med, 2020, 18(1):229. doi: 10.1186/s12916-020-01703-w [26] Lowe FJ, Luettich K, Gregg EO. Lung cancer biomarkers for the assessment of modified risk tobacco products: an oxidative stress perspective[J]. Biomarkers, 2013, 18(3):183-195. [27] 徐甜,殷文军,何芳,等.吸烟、白细胞计数与男性放射工作人员血清胆红素水平的关联性[J].公共卫生与预防医学,2021,32(1):67-71. doi: 10.3969/j.issn.1006-2483.2021.01.017 [28] Smith HA, Kang Y. The metastasis-promoting roles of tumor-associated immune cells[J]. J Mol Med (Berl), 2013, 91(4):411-429. doi: 10.1007/s00109-013-1021-5 [29] Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation[J]. Cell, 2011, 144(5):646-674. doi: 10.1016/j.cell.2011.02.013 [30] 钱香,王宏,任真.NLR与FIB和CEA及CA19-9在结直肠癌中的应用价值[J].中华预防医学杂志,2021,55(4):499-505. doi: 10.3760/cma.j.cn112150-20200805-01094 [31] Rocuts F, Zhang X, YanJ, et al. Bilirubin promotes de novo generation of T regulatory cells[J]. Cell Transplant, 2010, 19(4):443-451. doi: 10.3727/096368909X484680 [32] Neavin DR, Liu D, Ray B, et al. The role of the aryl hydrocarbon receptor (AHR) in immune and inflammatory diseases[J]. Int J Mol Sci, 2018, 19(12):3851. doi: 10.3390/ijms19123851 [33] 蔡春仙,付琪备,雷宇,等.C反应蛋白及直接胆红素作为肝细胞癌合并大血管侵袭的早期诊断指标[J].中华肝脏病杂志,2020,28(8):692-698. doi: 10.3760/cma.j.cn501113-20200619-00333 [34] Milkovic L, Siems W, Siems R, et al. Oxidative stress and antioxidants in carcinogenesis and integrative therapy of cancer[J]. Curr Pharm Des, 2014, 20(42):6529-6542. doi: 10.2174/1381612820666140826152822 [35] McCullough ML, Hodge RA, Campbell PT, et al. Pre-diagnostic circulating metabolites and colorectal cancer risk in the cancer prevention study-II nutrition cohort[J]. Metabolites, 2021, 11(3):156. doi: 10.3390/metabo11030156 -



 下载:
下载: