Comparison of safety and short-term efficacy between laparoscopy and laparotomy for locally advanced proximal gastric cancer after neoadjuvant chemotherapy
-
摘要:
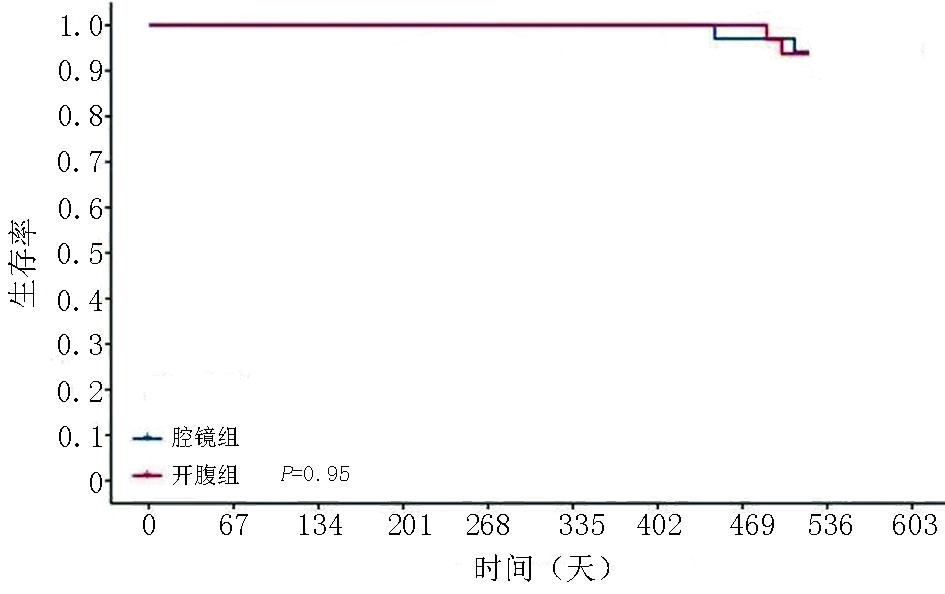
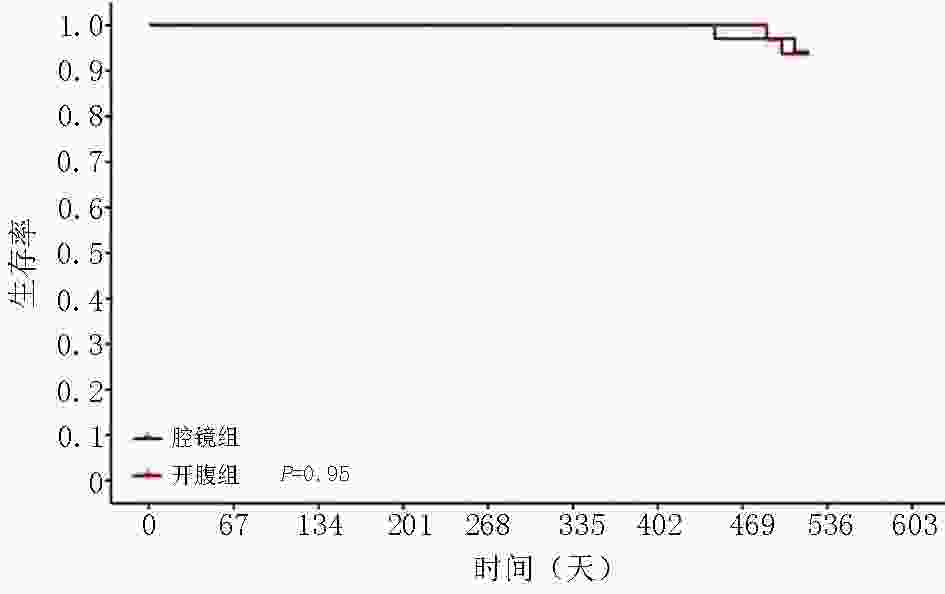
目的 研究局部进展期近端胃癌新辅助化疗后腹腔镜与开腹手术在安全性与近期疗效方面的差异。 方法 回顾性分析2018年1月至2020年1月徐州医科大学附属医院收治的74例局部进展期近端胃癌患者的临床资料。通过倾向性评分法进行1∶1匹配将66例患者纳入研究。新辅助化疗后,行腹腔镜手术患者34例,行开腹手术患者32例,比较两组患者的手术时间、术中出血量、淋巴结清扫数目、进食时间、术后住院天数及并发症,随访术后18个月患者的总生存期(overall survival,OS )及无病生存期(disease- free survival,DFS)。 结果 两组数据对比发现,腹腔镜手术在术中出血量、术后住院时间、排气时间及进食时间上更具优势,在手术时间、清扫淋巴结数目方面逊于开腹手术,差异有统计学意义(P<0.05);两组在术后并发症、18个月OS及DFS方面,差异无统计学意义(P>0.05)。 结论 腹腔镜手术能减少术中出血量及缩短术后恢复时间,但在手术时间及淋巴结清扫数目上逊于开腹手术;腔镜手术的安全性及近期疗效值得肯定,长期疗效值得进一步研究。 Abstract:Objectives To compare the safety and short-term curative effect of laparoscopic proximal gastrectomy (LPG) versus open proximal gastrectomy (OPG) in treating locally advanced proximal gastric cancer after neoadjuvant chemotherapy (NACT) and to investigate the rationality of surgical selection. Methods The clinical data of 74 patients admitted for locally advanced proximal gastric cancer at Affiliated Hospital of Xuzhou Medical University between January 2018 and January 2020 were retrospectively analyzed. Sixty-six patients were enrolled after 1:1 matching through the propensity scoring method. All received neoadjuvant chemotherapy preoperatively. Thirty-four patients were assigned into the laparoscopic group and 32 patients into the open group. For the safety of the two groups during the operation and intraoperative postoperative related-index analysis, specifically for the patients with some clinical indicators, such as operation time, amount of intraoperative blood loss, dissected lymph node numbe, postoperative intestinal function recovery time, postoperative hospitalization time, and postoperative complications, the 18-month overall survival (OS) and disease-free survival (DFS) rates. Results Laparoscopic surgery has more advantages with respect to the amount of intraoperative blood loss, postoperative hospital stay, exhaust time, and feeding time (P<0.05). However, the operation time was shorter and number of dissected lymph nodes was more in the open group than that in the laparoscopic group. Postoperative complications and the rate of the 18-month OS and DFS were not significantly different (P>0.05). Conclusions Laparoscopic surgery can reduce intraoperative blood loss and postoperative recovery time, but it is inferior to open surgery in operative time and number of lymph nodes dissected. The safety and short-term efficacy of laparoscopic surgery deserve affirmation and long-term efficacy should be further studied. -
Key words:
- neoadjuvant chemotherapy /
- laparoscopic /
- gastrectomy /
- advanced proximal gastric cancer
-
表 1 两组患者基本资料比较
项目 腹腔镜组(n=34) 开腹组(n=32) z/χ2值 P 性别 0.243 0.622 男 18 15 女 16 17 糖尿病史 9 8 0.019 0.891 高血压史 7 11 1.580 0.209 腹部手术史 3 4 0.235 0.628 ASA分级 −0.219 0.827 1 8 6 2 24 25 3 2 1 化疗方案 1.448 0.229 Flot 22 25 Sox 12 7 化疗周期 0.225 0.635 3 8 6 4 26 26 RECIST标准 1.436 0.151 完全缓解 1 0 部分缓解 27 22 稳定 6 10 疾病进展 0 0 表 2 两组患者肿瘤相关资料比较
项目 腹腔镜组(n=34) 开腹组(n=32) z/χ2值 P 肿瘤位置 −0.971 0.273 贲门 28 23 胃底 5 7 胃体 1 2 病理分型 −0.411 0.681 腺癌−高分化 2 1 腺癌−中分化 7 10 腺癌−低分化 21 17 印戒细胞癌 4 4 Lauren分型 −1.357 0.175 肠型 8 4 弥漫型 26 27 混合型 0 1 TRG评分 −1.300 0.194 0 1 0 1 6 4 2 23 21 3 4 7 肿瘤临床T分期 −1.133 0.257 T2 5 3 T3 24 21 T4 5 8 肿瘤临床N分期 −0.946 0.344 N0 8 6 N1 21 18 N2 5 8 肿瘤病理T分期 −0.032 0.975 T1 1 3 T2 3 2 T3 25 21 T4 5 6 肿瘤病理N分期 −1.626 0.104 N0 9 11 N1 10 13 N2 13 7 N3 2 1 表 3 手术根治性比较
项目 腹腔镜组(n=34) 开腹组(n=32) z/t/χ2值 P 近切端距离(cm) 3.8±1.5 3.8±1.1 0.103 0.918 远切端距离(cm) 14.8±3.9 15.6±4.7 −0.722 0.473 淋巴结清扫总数 21.7±3.8 25.0±4.8 −2.723 0.008 阳性淋巴结数 4.3(2,6) 4.2(1,6) −0.661 0.244 表 4 术中及术后观察指标
项目 腹腔镜组(n=34) 开腹组(n=32) z/t/χ2值 P 手术时间(min) 246.8±47.3 221.0±40.0 2.401 0.019 术中出血量(mL) 92(50,100) 121(92.5,130) −3.000 0.003 手术切口长度(cm) 8(6,9) 17(15.3,18) −7.053 <0.001 排气时间(d) 2.6(2,3) 3.4(3,4) −3.334 0.001 进食时间(d 5.4(5,7) 6.4(5,7) −2.724 0.005 引流管拔除时间(d) 8.2(7,9) 8.9(7,10.75) −1.114 0.265 住院时间(d) 11.5(10,13) 12.3(11,13.75) −1.411 0.158 术后并发症 −0.919 0.358 肺部感染 4 2 腹腔感染 1 1 切口感染 1 1 淋巴漏 1 1 术后出血 0 1 吻合口瘘 1 1 -
[1] TorreLA, Bray F, Siegel RL, et al. Global cancer statistics, 2012[J]. CA Cancer J Clin, 2015, 65:87-108. doi: 10.3322/caac.21262 [2] Wang FH, Zhang XT, Li YF, et al. The Chinese Society of Clinical Oncology (CSCO): clinical guidelines for the diagnosis and treatment of gastric cancer, 2021[J]. Cancer Commu (Lond), 2021, 41(8):49. [3] Wu LM, Jiang XJ, Lin QF, et al. Comparative study of clinical efficacy of laparoscopy-assisted radical gastrectomy versus open radical gastrectomy for advanced gastric cancer[J]. Genet Mol Res, 2015, 14(2):3459-3465. [4] Hu Y, Ying M, Huang C, et al. Oncologic outcomes of laparoscopy-assisted gastrectomy for advanced gastric cancer: a large-scale multicenter retrospective cohort study from China[J]. Surg Endosc, 2014, 28(7):2048-2056. doi: 10.1007/s00464-014-3426-9 [5] Yu J, Huang C, Sun Y, et al. Effect of laparoscopic vs open distal gastrectomy on 3-Year Disease-Free Survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial[J]. Transl Gastroenterol Hepatol, 2019, 321(20):1983-1992. [6] 赵东兵,张晓杰.膜解剖理念在新辅助治疗胃癌患者手术中的应用思考[J].中华胃肠外科杂志,2020,23(7):657-660. doi: 10.3760/cma.j.cn.441530-20200430-00249 [7] 左婷婷,郑荣寿,曾红梅,等.中国胃癌流行病学现状[J].中国肿瘤临床,2017,44(1):52-58. doi: 10.3969/j.issn.1000-8179.2017.01.881 [8] Hu Y, Huang C, Sun Y, et al. Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: arandomized controlled trial[J]. J Clin Oncol, 2016, 34(12):1350-1357. doi: 10.1200/JCO.2015.63.7215 [9] Li ZY, Shan F, Zhang LH, etal. Complications after radical gastrectomy following FOLFOX7 neoadjuvant chemotherapy for gastric cancer[J]. World J Surg Oncol, 2011, 26(9):110. [10] Coccolini F, Nardi M, Montori G, et al. Neoadjuvant chemotherapy in advanced gastric and esophago-gastric cancer. Meta-analysis of randomized trials[J]. Int J Surg, 2018, 51:120-127. doi: 10.1016/j.ijsu.2018.01.008 [11] Hosoda K, Katada C, Ishido K, et al. Neoadjuvant chemotherapy plus surgery for high-risk advanced gastric cancer: long-term results of KDOG1001 trial[J]. Langenbecks Arch Surg, 2020, 405(6):777-785. [12] Umeda S, Kanda M, NakanishiK, et al. Short-term outcomes of gastrectomy after neoadjuvant chemotherapy for clinical stage III gastric cancer: propensity score-matched analysis of a multi-institutional database[J]. Surg Today, 2021, 51(5):821-828. doi: 10.1007/s00595-020-02179-0 [13] Yan Y, Yang A, Lu L, et al. Impact of neoadjuvant therapy on minimally invasive surgical outcomes in advanced gastric cancer: an international propensity Score-Matched study[J]. Ann Surg Oncol, 2021, 28(3):1428-1436. doi: 10.1245/s10434-020-09070-9 [14] Li Z, Shan F, Ying X, et al. Assessment of laparoscopic distal gastrectomy after neoadjuvant chemotherapy for locally advanced gastric cancer: arandomized clinical trial[J]. JAMA Surg, 2019, 154(12):1093-1101. doi: 10.1001/jamasurg.2019.3473 [15] Li Z, Shan F, Ying X, et al. Laparoscopic or open distal gastrectomy after neoadjuvant chemotherapy for advanced gastric cancer: study protocol for a randomised phase II trial[J]. BMJ Open, 2018, 8(8):e021633. doi: 10.1136/bmjopen-2018-021633 [16] 陈起跃,钟情,刘治羽,等.腹腔镜进展期胃癌根治术在中国的进展[J].中国肿瘤临床,2021,48(3):110-117. [17] Tahara T, Shibata T, Okubo M, et al. Histological evaluations of primary lesions are independently associated with prognosis in patients with gastric cancer who receive neoadjuvant chemotherapy[J]. Oncol Lett, 2017, 13(6):4892-4896. [18] Xu X, Zheng G, Zhang T, et al. Is pathologic tumor regression grade after neo-adjuvant chemotherapy a promising prognostic indicator for patients with locally advanced gastric cancer? A cohort study evaluating tumor regression response[J]. Cancer Chemother Pharmacol, 2019, 84(3):635-646. doi: 10.1007/s00280-019-03893-4 [19] Mi SK, Lim JS, Hyung WJ, et al. Neoadjuvant chemoradiotherapy followed by D2 gastrectomy in locally advanced gastric cancer[J]. World J Gastroenterol, 2015, 21(9):2711-2718. doi: 10.3748/wjg.v21.i9.2711 [20] Qi X, Liu Y, Wang W, et al. Management of advanced gastric cancer: an overview of major findings from meta-analysis[J]. Oncotarget, 2016, 7(47):78180-78205. doi: 10.18632/oncotarget.12102 [21] Fujisaki M, Mitsumori N, Shinohara T, et al. Short- and long-term outcomes of laparoscopic versus open gastrectomy for locally advanced gastric cancer following neoadjuvant chemotherapy[J]. Surg Endosc, 2021, 35(4):1682-1690. doi: 10.1007/s00464-020-07552-1 -



 下载:
下载: