|
[1]
|
Forte D, García-Fernández M, Sánchez-Aguilera A, et al. Bone marrow mesenchymal stem cells support acute myeloid leukemia bioenergetics and enhance antioxidant defense and escape from chemotherapy[J]. Cell Metab, 2020, 32(5):829-843. doi: 10.1016/j.cmet.2020.09.001
|
|
[2]
|
Ji DX, He Y, Lu W, et al. Small-sized extracellular vesicles (EVs) derived from acute myeloid leukemia bone marrow mesenchymal stem cells transfer miR-26a-5p to promote acute myeloid leukemia cell proliferation, migration, and invasion[J]. Hum Cell, 2021, 34(3):965-976. doi: 10.1007/s13577-021-00501-7
|
|
[3]
|
Lawler J. The functions of thrombospondin-1 and-2[J]. Curr Opin Cell Biol, 2000, 12(5):634-640. doi: 10.1016/S0955-0674(00)00143-5
|
|
[4]
|
Adams JC. Thrombospondins: multifunctional regulators of cell interactions[J]. Annu Rev Cell Dev Biol, 2001, 17:25-51. doi: 10.1146/annurev.cellbio.17.1.25
|
|
[5]
|
Tian C, Li YY, Wang LN, et al. Blockade of FGF2/FGFR2 partially overcomes bone marrow mesenchymal stromal cells mediated progression of T-cell acute lymphoblastic leukaemia[J]. Cell Death Dis, 2022, 13(11):922. doi: 10.1038/s41419-022-05377-5
|
|
[6]
|
Chen ZH, Zheng YX, Yang YL, et al. Abnormal bone marrow microenvironment: the “harbor” of acute lymphoblastic leukemia cells[J]. Blood Sci, 2021, 3(2):29-34. doi: 10.1097/BS9.0000000000000071
|
|
[7]
|
Tian C, Zheng GG, Zhuang HQ, et al. MicroRNA-494 activation suppresses bone marrow stromal cell-mediated drug resistance in acute myeloid leukemia cells[J]. J Cell Physiol, 2017, 232(6):1387-1395. doi: 10.1002/jcp.25628
|
|
[8]
|
Carter BZ, Mak PY, Wang XM, et al. An ARC-regulated IL1β/cox-2/PGE2/β-catenin/ARC circuit controls leukemia-microenvironment interactions and confers drug resistance in AML[J]. Cancer Res, 2019, 79(6):1165-1177.
|
|
[9]
|
Azadniv M, Myers JR, McMurray HR, et al. Bone marrow mesenchymal stromal cells from acute myelogenous leukemia patients demonstrate adipogenic differentiation propensity with implications for leukemia cell support[J]. Leukemia, 2020, 34(2):391-403. doi: 10.1038/s41375-019-0568-8
|
|
[10]
|
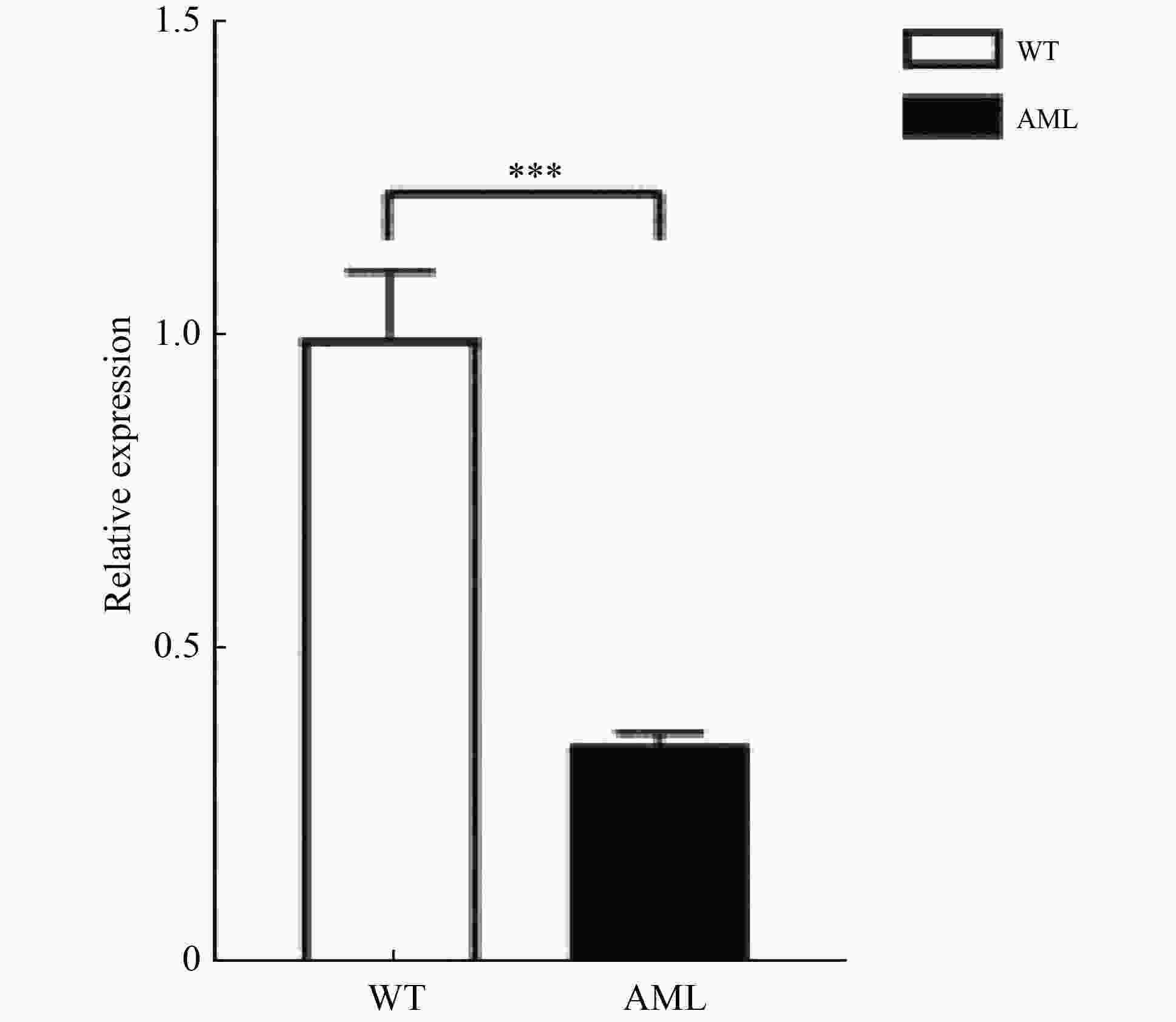
Zhu LD, Li Q, Wang XG, et al. THBS1 is a novel serum prognostic factors of acute myeloid leukemia[J]. Front Oncol, 2019, 9:1567.
|
|
[11]
|
Kaur S, Bronson SM, Pal-Nath D, et al. Functions of thrombospondin-1 in the tumor microenvironment[J]. Int J Mol Sci, 2021, 22(9):4570.
|
|
[12]
|
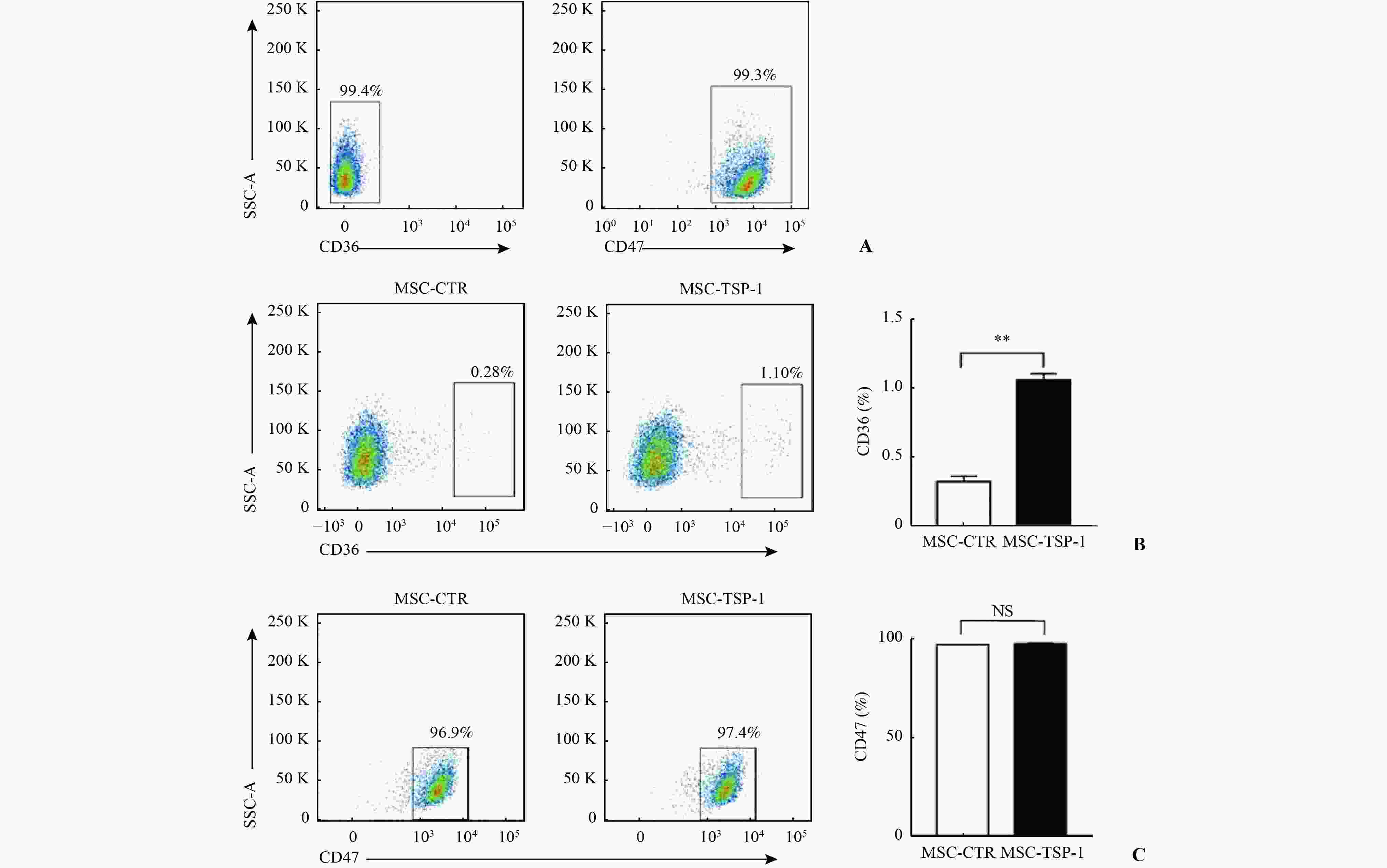
Wang JC, Li YS. CD36 tango in cancer: signaling pathways and functions[J]. Theranostics, 2019, 9(17):4893-4908. doi: 10.7150/thno.36037
|
|
[13]
|
Chu LY, Ramakrishnan DP, Silverstein RL. Thrombospondin-1 modulates VEGF signaling via CD36 by recruiting SHP-1 to VEGFR2 complex in microvascular endothelial cells[J]. Blood, 2013, 122(10):1822-1832.
|
|
[14]
|
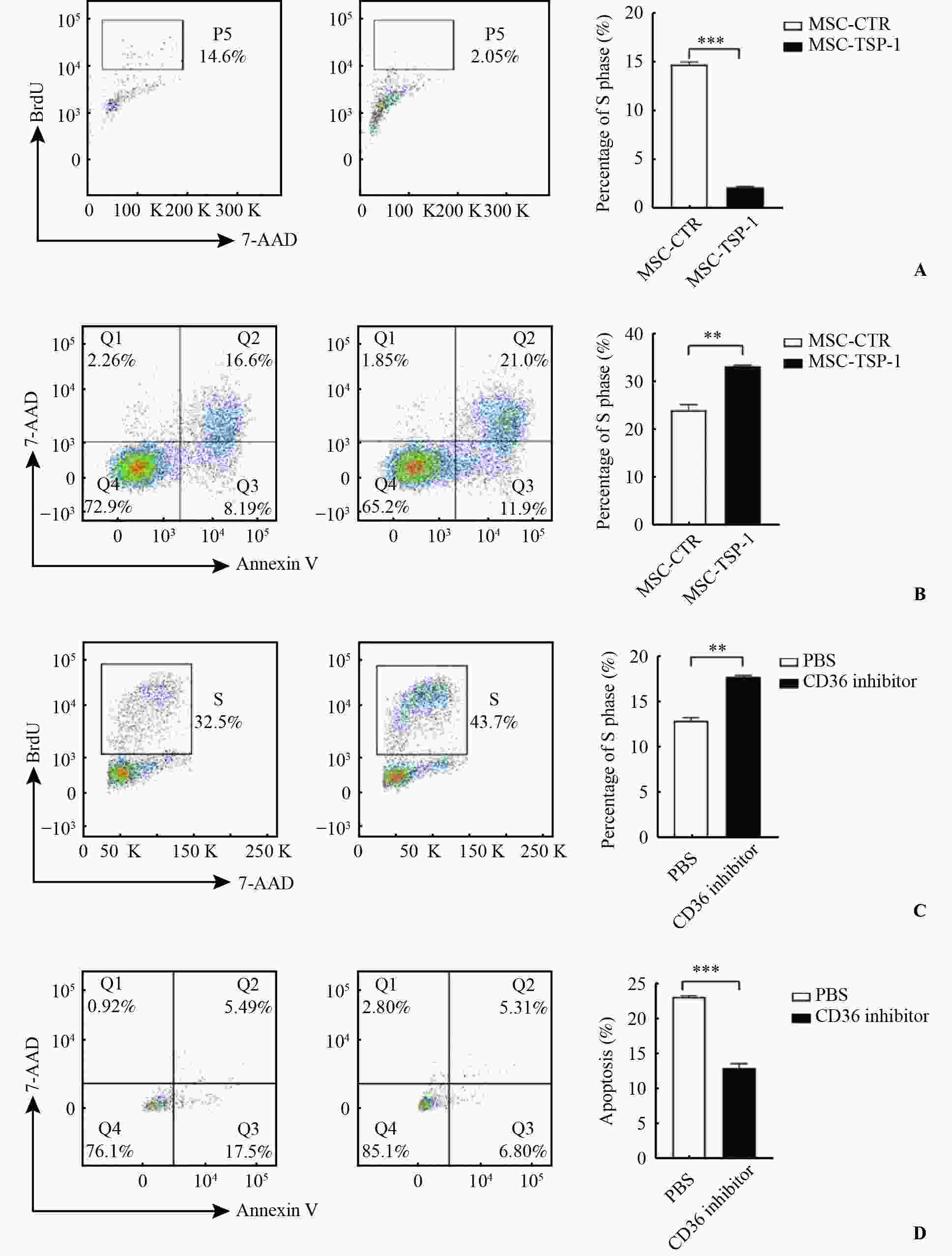
Li KR, Yang M, Yuen PM, et al. Thrombospondin-1 induces apoptosis in primary leukemia and cell lines mediated by CD36 and caspase-3[J]. Int J Mol Med, 2003, 12(6):995-1001.
|
|
[15]
|
Mateo V, Brown EJ, Biron G, et al. Mechanisms of CD47-induced caspase-independent cell death in normal and leukemic cells: link between phosphatidylserine exposure and cytoskeleton organization[J]. Blood, 2002, 100(8):2882-2890. doi: 10.1182/blood-2001-12-0217
|
|
[16]
|
Saumet A, Slimane MB, Lanotte M, et al. Type 3 repeat/C-terminal domain of thrombospondin-1 triggers caspase-independent cell death through CD47/alphavbeta3 in promyelocytic leukemia NB4 cells[J]. Blood, 2005, 106(2):658-667. doi: 10.1182/blood-2004-09-3585
|



 下载:
下载: