Analysis of the clinical application value of single-port inflatable endoscopy via axillary approach surgery for breast diseases
-
摘要:
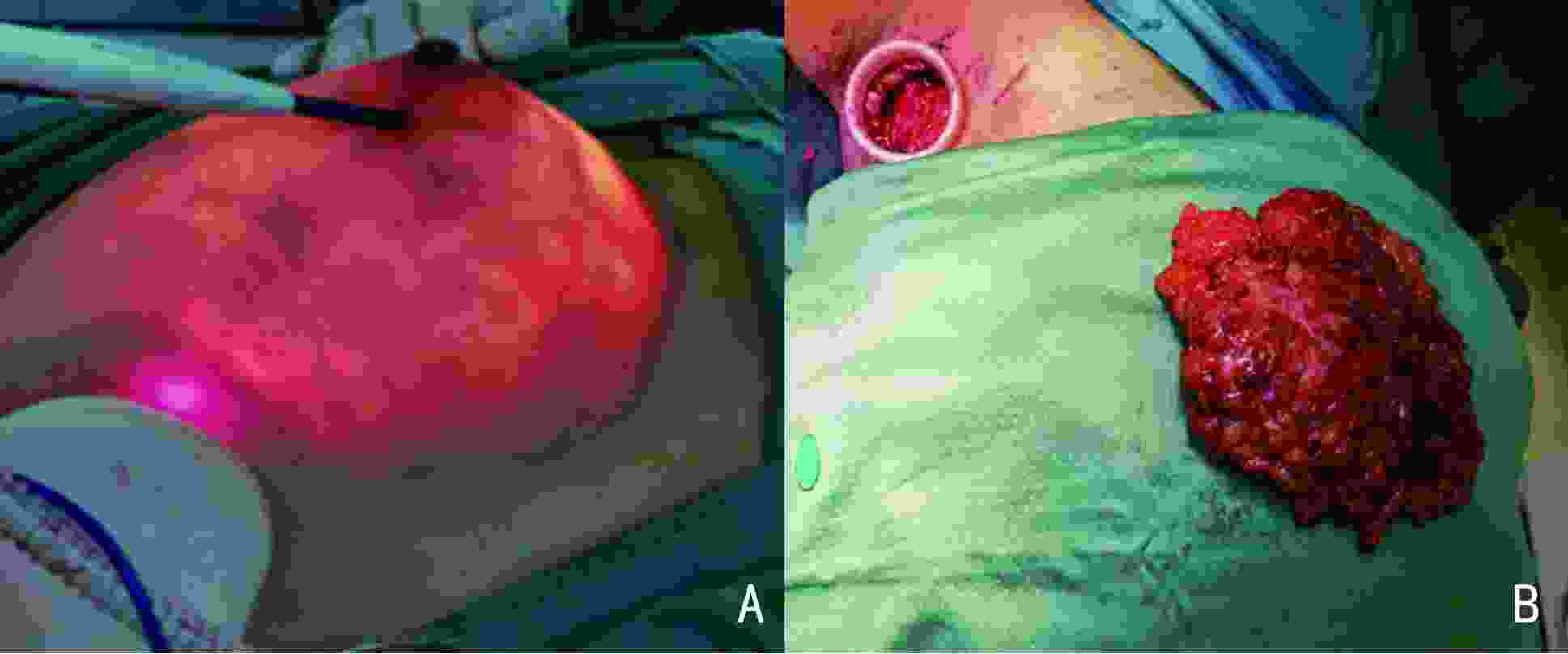
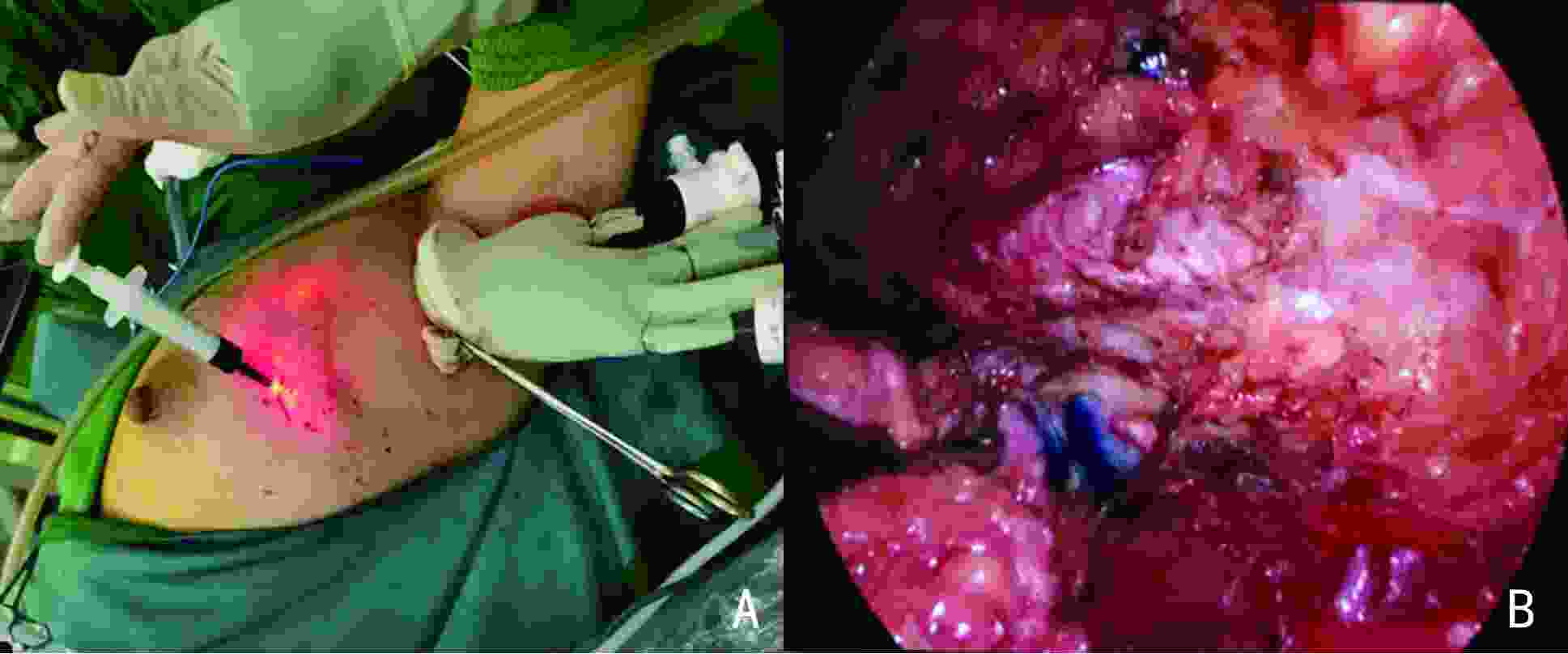
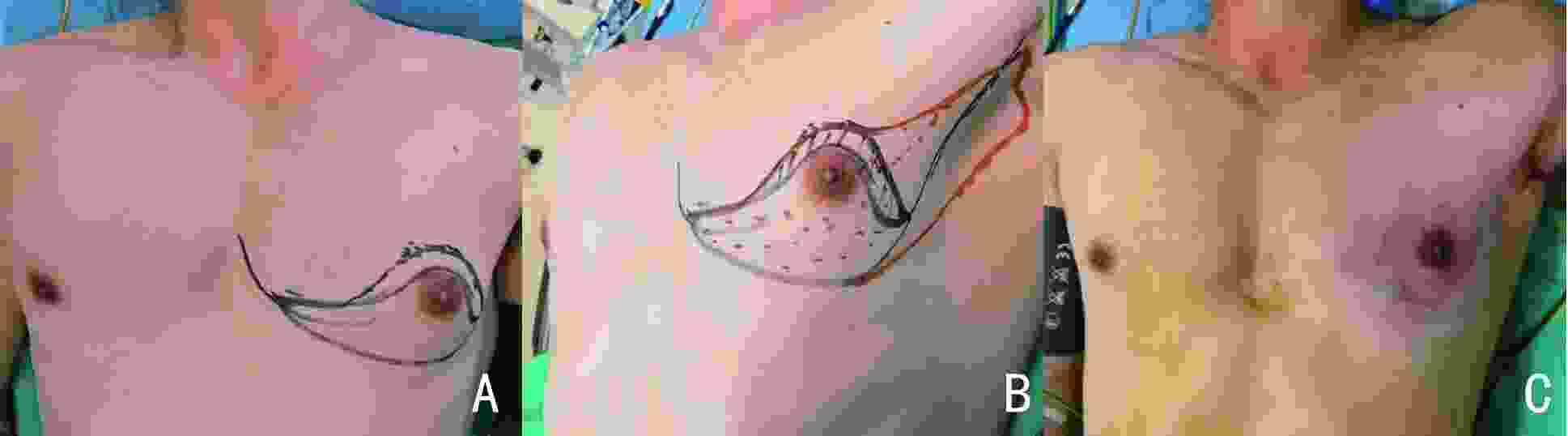
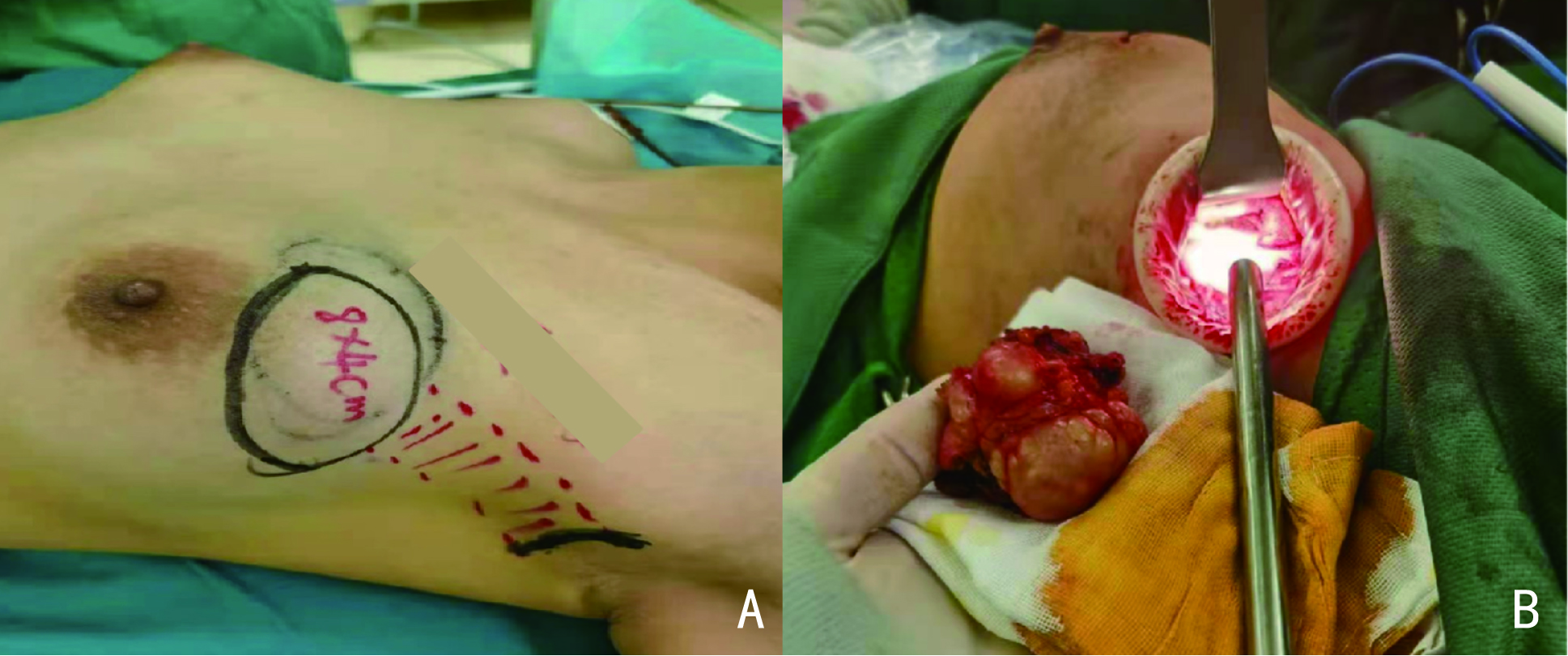
目的 探讨采用经腋窝单孔充气法乳腺腔镜手术在乳腺疾病中的可行性、安全性及临床应用价值。 方法 回顾性分析2020年12月至2022年3月于天津医科大学肿瘤医院收治经腋窝单孔充气法乳腺腔镜手术的84例乳腺疾病患者的临床资料,包括患者基线临床特征、术中及术后恢复情况、术后满意度评分及随访情况。 结果 84例患者均顺利完成手术,无中途转为开放手术病例。术后满意度评分为(8.25±1.21)分,手术效果佳。术后无切口感染、切缘坏死等重大并发症发生。随访8~23个月,未发现肿瘤局部复发及转移。 结论 经腋窝单孔充气法乳腺腔镜手术安全高效、并发症少、患者满意度高,临床应用上具有推广前景。 Abstract:Objective To explore the feasibility, safety and clinical application value of single-port inflatable endoscopic by the axillary approach in the treatment of breast diseases. Methods The clinical data of 84 patients with breast diseases received single-port inflatable endoscopic by the axillary approach breast surgery from December 2020 to March 2022 in Tianjin Medical University Cancer Institute & Hospital were analyzed retrospectively and followed up. The clinical characteristics, intraoperative and postoperative recovery, postoperative satisfaction scores, and local recurrence and distant metastasis were evaluated. Results The operations in 84 patients were successfully completed without the requirement for conversion to open surgery. The score of postoperative breast satisfaction was (8.25 $ \pm $ 1.21). There were no major complications such as incision infection and necrosis of incision margin after operation. During the follow-up period of 8–23 months, none of the patients showed local recurrence or tumor metastasis.Conclusions The single-port inflatable endoscopic by the axillary approach breast surgery is safe and efficient, with few complications and high patient satisfaction, and has a promising prospect in clinical application. -
Key words:
- breast neoplasm /
- endoscopy /
- prosthesis implantation
-
表 1 84例患者的一般临床资料
临床参数 例数(例) 百分比(%) 年龄(岁) 10~20 13 15.5 21~30 13 15.5 31~40 26 30.9 41~50 23 27.4 >50 9 10.7 性别 女 81 96.4 男 3 3.6 病变位置 左侧 44 52.4 右侧 37 44.0 双侧 3 3.6 肿瘤家族史 有 1 1.2 无 83 98.8 病理类型 导管内乳头状瘤 1 1.2 纤维瘤 17 20.2 良性叶状肿瘤 5 5.9 硬化性腺病 1 1.2 囊肿伴慢性炎症 1 1.2 男性乳腺发育腺体 3 3.6 导管原位癌 7 8.3 浸润性导管癌 38 45.2 浸润性小叶癌 3 3.6 浸润性乳头状癌 4 4.8 无病理结果(破裂假体取出) 4 4.8 患者生育史 有 58 69.1 无(含男性) 26 30.9 患者哺乳史 有 55 65.5 无(含男性) 29 34.5 吸烟史 有 6 8.2 无 78 91.8 表 2 84例患者围手术期相关情况
手术名称 例数
(例)平均年龄
(岁)平均手术时长
(min)清扫淋巴结
数量(枚)阳性淋巴结
数量(枚)术中出血量
(mL)引流量
(mL)引流时间
(天)肿物区段切除术 25 23.88±11.40 69.28±29.88 - - 32.20±18.82 26.08±9.78 3.36±1.29 全乳切除术+SLNB 6 44.50±10.92 105.00±15.00 8.17±4.98 0.17±0.37 50.83±26.21 101.67±26.09 5.33±1.37 全乳切除术+SLNB+ALND 7 42.29±8.56 170.00±35.96 17.14±5.67 0.71±0.88 95.71±7.28 125.71±19.35 5.86±0.83 全乳切除术+SLNB+Ⅰ期
假体重建术22 42.77±6.95 157.00±37.78 8.23±4.85 0.09±0.42 97.95±35.00 107.50±27.38 6.82±2.81 全乳切除术+SLNB+ALND+Ⅰ期
假体重建术7 40.43±7.15 178.57±34.40 15.00±4.66 2.43±1.68 121.43±52.49 100.71±19.54 6.86±1.96 全乳切除+SLNB+ALND+扩张器
置入术7 38.29±3.19 162.86±13.85 18.00±4.81 4.86±2.23 130.00±35.05 80.71±15.91 4.71±1.75 保乳术+SLNB 3 38.67±4.71 133.33±13.12 2.33±1.70 0.33±0.47 133.33±47.14 58.33±15.46 5.33±1.25 男性乳腺发育腺体切除术 3 20.67±5.44 79.33±17.02 - - 21.67±2.36 26.67±2.34 3.67±0.94 清创+假体取出术 4 54.75±6.98 102.15±15.80 - - 23.33±4.72 72.00±12.08 8.67±2.49 表 3 84例患者术后常见并发症发生情况
并发症 例数(例) 百分比(%) 切口感染 0 0 上肢水肿 3 3.6 伤口出血 1 1.2 皮下积液 1 1.2 术后疼痛 7 8.3 皮肤感觉异常 4 4.8 -
[1] Luo CY, Guo WB, Yang J, et al. Comparison of mastoscopic and conventional axillary lymph node dissection in breast cancer: long-term results from a randomized, multicenter trial[J]. Mayo Clin Proc, 2012, 87(12):1153-1161. doi: 10.1016/j.mayocp.2012.07.022 [2] Ngambenjawong C, Gustafson HH, Pun SH. Progress in tumor-associated macrophage (TAM)-targeted therapeutics[J]. Adv Drug Deliv Rev, 2017, 114:206-221. doi: 10.1016/j.addr.2017.04.010 [3] Wang ZH, Qu X, Teng CS, et al. Preliminary results for treatment of early stage breast cancer with endoscopic subcutaneous mastectomy combined with endoscopic sentinel lymph node biopsy in China[J]. J Surg Oncol, 2016, 113(6):616-620. doi: 10.1002/jso.24199 [4] Lim SML, Lam FL. Laparoscopic-assisted axillary dissection in breast cancer surgery[J]. Am J Surg, 2005, 190(4):641-643. [5] Yamashita K, Shimizu K. Video-assisted breast surgery: reconstruction after resection of more than 33% of the breast[J]. J Nippon Med Sch, 2006, 73(6):320-327. doi: 10.1272/jnms.73.320 [6] Yamashita K, Shimizu K. Trans-axillary retro-mammary gland route approach of video-assisted breast surgery can perform breast conserving surgery for cancers even in inner side of the breast[J]. Chin Med J (Engl), 2008, 121(20):1960-1964. doi: 10.1097/00029330-200810020-00002 [7] Langer I, Kocher T, Guller U, et al. Long-term outcomes of breast cancer patients after endoscopic axillary lymph node dissection: a prospective analysis of 52 patients[J]. Breast Cancer Res Treat, 2005, 90(1):85-91. doi: 10.1007/s10549-004-3268-6 [8] Aponte-Rueda ME, Saade Cárdenas RA, Saade Aure MJ. Endoscopic axillary dissection: a systematic review of the literature[J]. Breast, 2009, 18(3):150-158. doi: 10.1016/j.breast.2009.05.001 [9] Smith J, Sen S, Weeks RJ, et al. Promoter DNA hypermethylation and paradoxical gene activation[J]. Trends Cancer, 2020, 6(5):392-406. doi: 10.1016/j.trecan.2020.02.007 [10] Miranda Furtado CL, Dos Santos Luciano MC, Silva Santos RD, et al. Epidrugs: targeting epigenetic marks in cancer treatment[J]. Epigenetics, 2019, 14(12):1164-1176. doi: 10.1080/15592294.2019.1640546 [11] Malur S, Bechler J, Schneider A. Endoscopic axillary lymphadenectomy without prior liposuction in 100 patients with invasive breast cancer[J]. Surg Laparosc Endosc Percutan Tech, 2001, 11(1):38-41. [12] Brunt LM, Jones DB, Wu JS, et al. Endoscopic axillary lymph node dissection: an experimental study in human cadavers[J]. J Am Coll Surg, 1998, 187(2):158-163. doi: 10.1016/S1072-7515(98)00141-0 [13] Pusic AL, Cemal Y, Albornoz C, et al. Quality of life among breast cancer patients with lymphedema: a systematic review of patient-reported outcome instruments and outcomes[J]. J Cancer Surviv, 2013, 7(1):83-92. doi: 10.1007/s11764-012-0247-5 [14] Sakamoto N, Fukuma E, Teraoka K, et al. Local recurrence following treatment for breast cancer with an endoscopic nipple-sparing mastectomy[J]. Breast Cancer, 2016, 23(4):552-560. doi: 10.1007/s12282-015-0600-4 [15] Du JZ, Liang QK, Qi XW, et al. Endoscopic nipple sparing mastectomy with immediate implant-based reconstruction versus breast conserving surgery: a long-term study[J]. Sci Rep, 2017, 7:45636. doi: 10.1038/srep45636 -




 下载:
下载: