Clinicopathologic Characteristics and Prognosis of Breast Neuroendocrine Carcinoma: An analysis of 32 Cases
-
摘要:
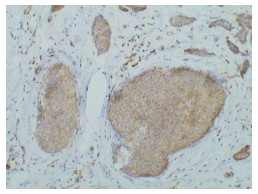
目的 探讨乳腺神经内分泌癌的临床病理特征及预后情况。 方法 回顾性分析天津医科大学附属肿瘤医院2003年1月~2010年7月收治的32例乳腺神经内分泌癌的临床特征、病理特点、治疗及预后。 结果 32例乳腺神经内分泌癌均为女性,均以无痛性乳腺肿物就诊,发病年龄36~76岁,(平均58.3岁)。病理检查具有神经内分泌癌的形态学特点,免疫组织化学染色结果突触素(synaptophysin)阳性率为54.5%(6/11),抗神经特异性烯醇化酶(NSE)阳性率为83.3%(20/24),嗜铬素A(CgA)阳性率为93.75%(30/32),ER阳性率为84.375%(27/32),PR阳性率为68.75%(22/32),C-erbB-2阳性率为9.375%(3/32),P53阳性率为18.75%(6/32)。随访时间7~91个月(平均30个月),除1例患者因全身多发转移死亡,1例患者出现骨转移,1例出现肺部多发转移,均带瘤生存外,余皆无瘤生存。ER与PR之间呈正相关关系(P < 0.01),且阳性表达率较高;ER、PR均与P53呈负相关关系(P < 0.01、P < 0.05),P53阳性表达率较低。单纯乳腺神经内分泌癌与伴有其他类型癌的乳腺神经内分泌癌相比,在TNM分期中二者具有明显的差异,且有统计学意义(P < 0.05)。13例伴有其他类型癌的乳腺神经内分泌癌均为高级别的TNM分期,而19例单纯乳腺神经内分泌癌却均为低级别TNM分期。 结论 乳腺神经内分泌癌是一类少见的特殊类型乳腺癌,病理形态复杂,免疫组织化学染色检测神经内分泌指标是确诊该病的可靠依据。综合治疗有利于提高患者的生存率,延长无病生存时间。本研究提示乳腺神经内分泌癌多为雌孕激素依赖性乳腺癌,可接受内分泌治疗。单纯乳腺神经内分泌癌的TNM分期相对较低,不易发生淋巴结转移,预后较好。仍需大样本长时间随访观察以得出有关乳腺神经内分泌癌的生物学行为及预后的可靠结论。 Abstract:Objective To study the clinicopathologic features and prognosis of breast neuroendocrine carcinoma (NEC). Methods Thirty-two breast NEC patients were admitted between January 2003 and July 2010 to Tianjin Medical University Cancer Institute and Hospital. Their clinicopathologic data, treatment, and prognosis were retrospectively analyzed. Results All of the 32 patients were females aged 36 years to 76 years (mean of 58.3 years), all 32 carcinomas were palpable, painless, and detected by the patients themselves. All cases were pathologically diagnosed as NEC. The immunohistochemical results showed that the positive rates for synaptophysin, NSE, and chromogranin A were 54.5% (6/11), 83.3% (20/24), and 93.75% (30/32), respectively. Twenty-seven cases were positive for ER, 22 for PR, 3 for C-erbB-2, and 6 for P53. All patients survived and were followed up for 7 to 91 months (mean of 30 months) except for one who died because of systemic multiple metastases. A positive correlation was observed between ER and PR (P < 0.01), and the positive rates for ER and PR were quite high. Moreover, both ER and PR were negatively correlated with P53 (P < 0.01 andP < 0.05, respectively) and had low positive expression. A significant difference was observed between the breast NEC simplex and complex in TNM staging (P < 0.05). All of the 13 cases of breast NEC complex had high TNM staging, whereas none of the 19 cases of breast NEC simplex had high TNM staging. Conclusion Breast NEC is a rare and distinct category with different histological subtypes. The diagnosis of this disease should depend on the neuroendocrine markers detected by immunohistochemistry. The combined treatment is valuable for improving the overall and disease-free survival rates. Breast NEC is mostly ER and/or PR dependent and can be treated with endocrine therapy. Breast NEC simplex has relatively low TNM staging and will not easily transfer to the lymph nodes, indicating a good prognosis. Larger samples and longer follow-up periods are needed to investigate the biological characteristics and prognosis of NEC. -
Key words:
- Breast /
- Neuroendocrine carcinoma (NEC) /
- Clinicopathological characteristic /
- Prognosis
-
表 1 32例单纯乳腺神经内分泌癌与伴随其他类型的乳腺神经内分泌癌的临床和病理比较
Table 1. The clinical and pathological features of 32 neuroendocrine carcinoma simplex of breast and the neuroendocrine carcinoma complex of breast

-
[1] Tavassoli FA, Devile P. WHO classification of tumours, pothogy and genetic of the breast and female organs[M]. Lyon: IARC, 2003: 32-34. [2] Sapino A, Righi L, Cassoni P, et al. Expression of the neuroendocrine phenotype in carcinomas of the breast[J]. Semin Diagn Pathol, 2000, 17(2): 127-137. http://www.ncbi.nlm.nih.gov/pubmed/10839613 [3] Maluf HM, Koerner FC. Carcinomas of the breast with endocrine differentiation: a review[J]. Virchows Arch, 1994, 425(5): 449-457. http://eurekamag.com/pdf/008/008264752.pdf [4] Sapino A, Righi L, Cassoni P, et al. Expression of apocrine differentiation markers in neuroendocrine breast carcinomas of aged women[J]. Mod Pathol, 2001, 14(8): 768-776. doi: 10.1038/modpathol.3880387 [5] Zekioglu O, Erhan Y, Ciris M, et al. Neuroendocrine differentiated carcinomas of the breast: a distinct entity[J]. Breast, 2003, 12(4): 251-257. doi: 10.1016/S0960-9776(03)00059-6 [6] Hennessy BT, Gilcrease MZ, Kim E, et al. Breast carcinoma with neuroendocrine differentiation and myocardial metastases[J]. Clin Breast Cancer, 2007, 7(11): 892-894. doi: 10.3816/CBC.2007.n.056 [7] Kawasaki T, Nakamura S, Sakamoto G, et al. Neuroendocrine ductal carcinoma in situ of the breast: cytological features in 32 cases[J]. Cytopathology, 2011, 22(1): 43-49. doi: 10.1111/j.1365-2303.2010.00742.x [8] Kawasaki T, Nakamura S, Sakamoto G, et al. Neuroendocrine ductal carcinoma in situ (NE-DCIS) of the breast--comparative clinicopathological study of 20 NE-DCIS cases and 274 non-NE-DCIS cases[J]. Histopathology, 2008, 53(3): 288-298. doi: 10.1111/j.1365-2559.2008.03093.x [9] Horiguchi S, Hishima T, Hayashi Y, et al. HER-2/neu cytoplasmic staining is correlated with neuroendocrine differentiation in breast carcinoma[J]. J Med Dent Sci, 2010, 57(2): 155-163. http://www.researchgate.net/profile/Yoshinobu_Eishi/publication/47788590_HER-2neu_cytoplasmic_staining_is_correlated_with_neuroendocrine_differentiation_in_breast_carcinoma/links/02bfe513e702eb3c06000000.pdf [10] Wei B, Ding T, Xing Y, et al. Invasive neuroendocrine carcinoma of the breast: a distinctive subtype of aggressive mammary carcinoma[J]. Cancer, 2010, 116(19): 4463-4473. doi: 10.1002/cncr.25352 [11] 崔明, 张霁, 冷家骅, 等. 乳腺小细胞神经内分泌癌(附3例报告) [J]. 中国实用外科杂志, 2008, 28(7): 550-552. doi: 10.3321/j.issn:1005-2208.2008.07.015 [12] Lee WS, Lee JE, Kim JH, et al. Analysis of prognostic factors and treatment modality changes in breast cancer: a single institution study in Korea[J]. Yonsei Med J, 2007, 48(3): 465-473. doi: 10.3349/ymj.2007.48.3.465 [13] 李琼, 王虹, 包芸, 等. 乳腺神经内分泌癌35例临床病理分析[J]. 复旦大学学报(医学版), 2008, 35(2): 247-251. https://www.cnki.com.cn/Article/CJFDTOTAL-SHYK200802023.htm [14] Rovera F, Masciocchi P, Coglitore A, et al. Neuroendocrine carcinomas of the breast[J]. Int J Surg, 2008, 6 Suppl 1: S113-S115. http://www.onacademic.com/detail/journal_1000035626313110_becd.html -




 下载:
下载: