Clinicopathologic Features and Prognosis of T1a and T1b Triple-Negative Breast Cancer
-
摘要:
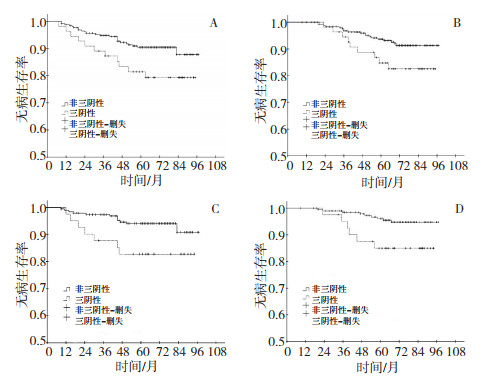
目的 分析小肿块(直径≤1 cm)乳腺癌患者的临床及病理学特征,了解其生存状态,探讨三阴性对其预后的影响。 方法 收集本院收治的312例直径≤1 cm乳腺癌患者的临床病理学资料,比较三阴性乳腺癌及非三阴性乳腺癌的临床病理学特征、复发转移及生存情况。 结果 312例直径≤1 cm乳腺癌患者纳入研究,三阴组及非三阴组5年DFS分别为81.4%及90.5%(P= 0.038),5年BCSS分别为84.7%及93.7%(P=0.047)。以淋巴结状态分组比较,淋巴结阴性患者中,三阴组及非三阴组5年DFS分别为82.8%及94.1%(P=0.033),5年BCSS分别为85.0%及96.1%(P=0.019)。Cox比例风险模型多因素分析显示,淋巴结阳性患者复发转移风险增高(HR=3.721,95%CI:1.743~7.941,P=0.001),死亡风险亦增高(HR=3.560,95%CI:1.521~8.330,P=0.003),三阴性患者复发转移风险增高(HR=2.208,95%CI:1.028~4.742,P=0.042)。 结论 淋巴结阳性及三阴性是影响直径≤1 cm乳腺癌患者DFS的独立危险因素,淋巴结阳性是影响BCSS的唯一独立危险因素。淋巴结阴性三阴性乳腺癌组较非三阴组预后差。 Abstract:Objective The aim of this study is to analyze the clinicopathological features and survival for patients with a tumor size ≤1 cm, and to clarify the prognostic significance of triple-negative breast cancer (TNBC). Methods Data from 312 patients with operable primary breast cancer with tumor size ≤1 cm, who were admitted to the Tianjin Medical University Cancer Institute and Hospital from January 2002 to June 2005, were gathered and analyzed, and the clinicopathological features, recurrence, metastasis, and survival status between TNBC and non-TNBC patients were compared. SPSS17.0 software was used for statistical analysis, with statistical significance considered at P < 0.05. Results The rates of 5-year disease-free survival (DFS) and breast cancer-specific survival (BCSS) of the TNBC patients were 81.4% and 84.7%, respectively, lower than those of the non-TNBC patients (P = 0.038; P = 0.047). In the lymph node-negative patients, the rates of 5-year DFS and BCSS of the TNBC patients were 82.8% and 85.0%, respectively, lower than those of the non-TNBC patients (P = 0.033; P = 0.019). In the multivariate Cox regression hazard analysis, lymph node infiltration was associated with a higher hazard ratio (HR) for disease recurrence (HR: 3.721, 95% CI: 1.743-7.941, P = 0.001), and BCSS (HR: 3.560, 95% CI: 1.521-8.330, P = 0.003). The TNBC group was associated with a higher HR for tumor recurrence (HR: 2.208, 95% CI: 1.028-4.742, P = 0.042) compared with the non-TNBC group. Conclusion Lymph node status and TNBC are independent prognostic factors for the recurrence and metastasis of tumor, while lymph node infiltration is the single independent prognostic factor for BCSS. TNBC can be an independent risk factor for T1a and T1b node-negative invasive breast cancer. -
Key words:
- Triple-negative breast cancer /
- Tumor size /
- Prognosis
-
表 1 三阴性与非三阴性直径≤1 cm乳腺癌患者的临床病理特征比较
Table 1. Comparison of clinicopathological features between TNBC and non-TNBC patients with tumor size ≤1 cm

表 2 影响DFS及BCSS的Cox比例风险回归单因素及多因素分析
Table 2. Univariate and multivariate Cox regression analysis for DFS and BCSS

表 3 不同组别乳腺癌患者化疗比率、5年DFS及BCSS比较
Table 3. Proportion of chemotherapy, 5-year DFS, and BCSS in patients of different groups

-
[1] Benson JR, Jatoi I, Keisch M, et al. Early breast cancer[J]. Lancet, 2009, 373: 1463-1479. doi: 10.1016/S0140-6736(09)60316-0 [2] Dent R, Trudeau M, Pritchard KI, et al. Triple- negative breast cancer: clinical features and patterns of recurrence[J]. Clin Cancer Res, 2007, 13: 4429-4434. doi: 10.1158/1078-0432.CCR-06-3045 [3] Sánchez-Muñoz A, Pérez-Ruiz E, Jurado JM. Outcome of small invasive breast cancer with no axillary lymph node involvement[J]. Breast J. 2011, 17(1): 32-38. doi: 10.1111/j.1524-4741.2010.01026.x [4] Cleator S, Heller W, Coombes RC. Triple-negative breast cancer: therapeutic options[J]. Lancet Oncol, 2007, 8(3): 235-244. doi: 10.1016/S1470-2045(07)70074-8 [5] Smart CR, Byrne C, Smith RA, et al. Twenty-year follow-up of the breast cancers diagnosed during the Breast Cancer Detection Demonstration Project[J]. CA Cancer J Clin, 1997, 47(3): 134-149. doi: 10.3322/canjclin.47.3.134 [6] Chen YY, Schnitt SJ. Prognostic factors for patients with breast cancers 1cm and smaller[J]. Breast Cancer Res Treat, 1998, 51(3): 209-225. doi: 10.1023/A:1006130911110 [7] Leitner SP, Swern AS, Weinberger D, et al. Predictors of recurrence for patients with small (one centimeter or less) localized breast cancer (T1a, bN0M0)[J]. Cancer, 1995, 76: 2266-2274. doi: 10.1002/1097-0142(19951201)76:11<2266::AID-CNCR2820761114>3.0.CO;2-T [8] Kwon JH, Kim YJ, Lee KW, et al. Triple negativity and young age as prognostic factors in lymph node-negative invasive ductal carcinoma of 1 cm or less[J]. BMC Cancer, 2010, 10: 557-564. doi: 10.1186/1471-2407-10-557 [9] Park YH, Kim ST, Cho EY, et al. A risk stratification by hormonal receptors (ER, PgR) and HER-2 status in small (< or = 1 cm) invasive breast cancer: who might be possible candidates for adjuvant treatment[J]? Breast Cancer Res Treat, 2010, 119(3): 653-661. doi: 10.1007/s10549-009-0665-x [10] Cancello G, Maisonneuve P, Rotmensz N, et al. Prognosis in women with small (T1mic, T1a, T1b) node-negative operable breast cancer by immunohistochemically selected subtypes[J]. Breast Cancer Res Treat, 2011, 127(3): 713-720. doi: 10.1007/s10549-011-1465-7 [11] Chia SK, Speers CH, Bryce CJ, et al. Ten-year outcomes in a population-based cohort of node-negative, lymphatic, and vascular invasion-negative early breast cancers without adjuvant systemic therapies[J]. J Clin Oncol, 2004, 22: 1630-1637. doi: 10.1200/JCO.2004.09.070 [12] Hassett MJ, Hughes ME, Niland JC, et al. Chemotherapy use for hormone receptor-positive, lymph node-negative breast cancer[J]. J Clin Oncol, 2008, 26(34): 5553-5560. doi: 10.1200/JCO.2008.17.9705 [13] Elder EE, Hay SB, Moore K. Factors Influencing Treatment Recommendations in Node-Negative Breast Cancer[J]. J Oncol Pract, 2011, 7(1): 26-30. doi: 10.1200/JOP.2010.000024 [14] Goldhirsch A, Ingle JN, Gelber RD, et al. Thresholds for therapies: highlights of the St Gallen International Expert Consensus on the primary therapy of early breast cancer 2009[J]. Ann Oncol, 2009, 20 (8): 1319-1329. doi: 10.1093/annonc/mdp322 -




 下载:
下载: