-
摘要:
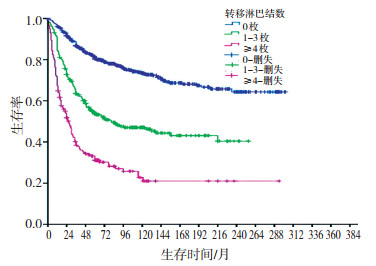
目的 研究我国不同TNM分期的结直肠癌治疗后的生存情况及其影响因素,以帮助判断预后。 方法 使用SPSS 19.0软件对1985年1月至2005年12月间于浙江大学医学院附属第二医院经手术病理证实的1 368例结直肠癌患者的19个临床及病理因素进行分析,单因素分析时采用Kaplan-Meier法计算生存率,Log-rank法比较生存率差异。多因素分析时采用Cox风险比例模型,得出影响结直肠癌患者预后的独立因素。按AJCC第七版TNM分期标准,对所有患者进行分期。 结果 1 368例患者3、5、10年总生存率分别为67.5%、60.2%、53.5%;根治术后3、5、10年生存率分别为77.6%、69.9%、62.4%。按AJCC第七版TNM分期,Ⅰ、Ⅱ、Ⅲ、Ⅳ期的5年生存率分别为90.1%、72.6%、53.8%、10.4%。Cox模型多因素分析发现肿瘤浸润深度、转移淋巴结数、送检淋巴结总数、邻近器官受累、远处转移、手术方式和术后感染等7个因素是影响结直肠癌预后的主要独立因素。尤其是ⅡC期患者的5年生存率(44.8%)低于ⅢA期(79.6%)、ⅢB期(58.0%),上述各因素的生存曲线比较其差异有统计学意义(P < 0.05)。 结论 肿瘤浸润深度、转移淋巴结数、送检标本淋巴结总数、邻近器官受累、远处转移、手术方式和术后感染等7个因素是影响结直肠癌预后的主要独立因素。原发肿瘤的浸润深度对于Ⅱ/Ⅲ期结直肠癌患者的预后可能更有提示作用。 Abstract:Objective To assess the survival rates of patients with different TNM stages, and to explore the prognostic factors of colorectal cancer. Methods A total of 1, 368 cases of colorectal cancer operated and pathologically confirmed at the Second Affiliated Hospital of Zhejiang University School of Medicine from 1985 to 2005 were collected. All cancers were pathologically staged according to AJCC TNM classification (seventh edition). Univariate and multivariate analyses were applied to evaluate the prognostic factors. For univariate analysis, the cumulative survival rate was calculated using the Kaplan-Meier method, and the significant difference was evaluated by the log-rank test. Cox multivariate regression analysis was performed to identify the predictors of survival. All these analyses were conducted using SPSS software (version 19.0). Results The 3-, 5-, and 10- year overalll survival rates were 67.5%, 60.2%, and 53%, respectively. The survival rates for 3, 5, and 10 years after radical resection were 77.6%, 69.9%, and 62.4% respectively. According to the TNM classification, the 5-year survival rates of the stage-Ⅰ, -Ⅱ, -Ⅲ, and -Ⅳ patients were 90.1%, 72.6%, 53.8%, and 10.4%, respectively. Multivariate analysis by Cox regression revealed that the following factors were independently associated with the cumulative survival rate of colorectal cancer: depth of invasion, lymph node metastasis, total number of lymph nodes, adjacent organ involvement, metastasis, radical resection, and post-operative infection. The 5-year overall survival rate was lower in stage-ⅡC patients than in stage-ⅢA or -ⅢB patients. The survival curves of the above factors were significantly different (P < 0.05). Conclusion The depth of invasion, lymph node metastasis, total number of lymph nodes inspected after surgery, adjacent organ involvement, metastasis, radical resection, postoperative infection are the independent prognostic factors of colorectal cancer. The depth of invasion may be a more precise prognostic factor for stage-Ⅱ and -Ⅲ patients. -
Key words:
- Colorectal cancer /
- Lymph node metastasis /
- TNM classification /
- Metastasis /
- Survival analysis
-
表 1 1 368例结直肠癌患者多因素Cox回归分析结果
Table 1. Result of Cox regression analysis for 1, 368 cases of colorectal cancer patients

表 2 各预后因素与相应的生存率
(x±s) Table 2. Prognostic factors and correlative survival rates

表 3 Ⅱ/Ⅲ期结直肠癌患者生存率
(x±s) Table 3. Survival rates of colorectal cancer patients with stage Ⅱ/Ⅲ

表 4 Log-rank法成对比较Ⅱ/Ⅲ期结直肠癌各亚群生存率的P值情况
Table 4. Survival evaluation for stage Ⅱ/Ⅲ clorectal cancer patients using Log-Rank test

-
[1] Jemal A, Bray F, Center MM, et al. Global cancer statistics[J]. CA Cancer J Clin, 2011, 61(2): 69-90. doi: 10.3322/caac.20107 [2] 雷涛, 陈万青, 张思维, 等. 1988-2002年中国10个市县结直肠癌的流行特征[J]. 中华肿瘤杂志, 2009, 31(6): 428-433. doi: 10.3760/cma.j.issn.0253-3766.2009.06.007 [3] Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011: The impact of eliminating socioeconomic and racial disparities on premature cancer deaths[J]. CA Cancer J Clin, 2011, 61(4): 212-236. doi: 10.3322/caac.20121 [4] Park YJ, Park KJ, Park JG, et al. Prognostic factors in 2230 Korean colorectal cancer patients: analysis of consecutively operated cases [J]. World J Surg, 1999, 23(7): 721-726. doi: 10.1007/PL00012376 [5] Ratto C, Sofo L, Ippoliti M, et al. Prognostic factors in colorectal cancer. Literature review for clinical application[J]. Dis Colon Rectum, 1998, 41(8): 1033-1049. doi: 10.1007/BF02237397 [6] 梁君林, 万德森, 潘志忠, 等. 结直肠癌根治术后复发转移的多因素分析[J]. 癌症, 2004, 23: 564-567. https://www.cnki.com.cn/Article/CJFDTOTAL-AIZH200405016.htm [7] 汪建平, 杨祖立, 王磊, 等. 结直肠癌临床病理特征与预后的多因素回归分析[J]. 中华肿瘤杂志, 2003, 25(1): 59-61. doi: 10.3760/j.issn:0253-3766.2003.01.015 [8] 刘彦龙, 赵发林, 王锡山. 2414例直肠癌患者的临床病理特征及预后分析[J]. 中华胃肠外科杂志, 2010, 13(12): 913-916. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWCW200406004.htm [9] Le Voyer TE, Sigurdson ER, Hanlon AL, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089[J]. J Clin Oncol, 2003, 21(15): 2912-2919. doi: 10.1200/JCO.2003.05.062 [10] Freedman LS, Macaskill P, Smith AN. Multivariate analysis of prognostic factors for operable rectal cancer[J]. Lancet, 1984, 2(8405): 733-736. http://www.onacademic.com/detail/journal_1000036179200610_be78.html [11] Akasu T, Yamaguchi T, Fujimoto Y, et al. Abdominal sacral resection for posterior pelvic recurrence of rectal carcinoma: analyses of prognostic factors and recurrence patterns[J]. Ann Surg Oncol, 2007, 14(1): 74-83. http://www.onacademic.com/detail/journal_1000034847939410_ae54.html [12] Rizk NP, Bach PB, Schrag D, et al. The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma[J]. J Am Coll Surg, 2004, 198(1): 42-50. doi: 10.1016/j.jamcollsurg.2003.08.007 [13] 郑树, 张苏展, 蔡善荣, 等. 结直肠癌筛查方案及其实践[J]. 中国肿瘤, 2009, 18(9): 700-704. [14] Mori T. A comparison of the new (planned) TNM classification and Japanese general rule for staging colorectal cancer[J]. Cancer Invest, 2010, 28: 387-392. doi: 10.1080/07357900903287055 [15] Lu AT, Salpeter SR, Reeve AE, et al. Gene expression profiles as predictors of poor outcomes in stage Ⅱ colorectal cancer: A systematic review and meta-analysis[J]. Clin Colorectal Cancer, 2009, 8: 207-214. doi: 10.3816/CCC.2009.n.035 [16] Yu SJ, Yu JK, Ge WT, et al. SPARCL1, Shp2, MSH2, E-cadherin, p53, ADCY-2 and MAPK are prognosis-related in colorectal cancer[J]. World J Gastroenterol, 2011, 17: 2028-2036. doi: 10.3748/wjg.v17.i15.2028 -




 下载:
下载: