Clinical diagnosis and analysis of primary pulmonary mucosa-as-sociated lymphoid tissue lymphoma: A report of seven cases
-
摘要:
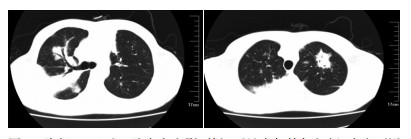
目的 探讨肺黏膜相关淋巴组织样淋巴瘤(mucosa associated lymphoid tissue,MALT)临床、病理特点,诊断及治疗。 方法 回顾7例肺MALT患者临床资料,结合文献对其临床及病理特点、免疫组织化学(CD20,CD79a,CD5,CD10,CD23,CyclinD1,Ki-67等)、诊断等进行总结分析。 结果 7例患者男3例、女4例,男女比例:1 :1.3。平均年龄58岁。4例患者存在吸烟、肺部反复感染等慢性免疫系统刺激因素。无症状体检发现者2例,余患者主要表现为:咳嗽、气促及不规则发热。胸部影像学表现为多发性浸润病变,双肺多发者4例,右肺者3例,胸腔积液5例。所有患者均呈CD19(+),CD20(+)。Ki-67阳性率较低。CD5、CD10、CyclinD1阴性。 结论 肺MALT大多数临床及影像学表现缺乏特异性,误诊率高,确诊依赖于组织病理学检查。关键词肺淋巴瘤粘膜相关淋巴样组织诊断 Abstract:Objective This study aims to examine the clinicopathological features, diagnosis, and treatment of pulmonary marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue (PMZL-MALT). Methods The clinicopathological features and immunohistochemical staining of CD20, CD79a, CD5, CD10, CD23, CyclinD1, and Ki-67 in seven patients with PMZL-MALT were analyzed. Results These patients, with a median age of 58 years, included three males and four females. Most of the patients suffered from cough, anhelation, and irregular fever. No specific imaging manifestation was observed. Tumor cells were positive for CD19 and CD20 but negative for CD5, CD10, and CyclinD1. The positive rate of Ki-67 was low. Conclusion PMZL-MALT cases are easily misdiagnosed because of the absence of specific clinical characteristics and X-ray features. Final diagnosis depends on pathological examinations. -
Key words:
- pulmonary /
- lymphoma /
- mucosa-associated lymphoid tissue /
- diagnosis
-
表 1 Ann Arbor肺部淋巴瘤分期
Table 1. Ann Arbor stages of primary pulmonary lymphoma

-
[1] Ferraro P, Trastek VF, Adlakha H, et al. Primary non-Hodgkin's lymphoma of the lung[J]. Ann Thorac Surg, 2000, 69(4):993-997. doi: 10.1016/S0003-4975(99)01535-0 [2] Burke JS. Are there site-specific differences among the MALT lym phoma-morphologic, clinical[J]? Am J Clin Pathol, 1999, 111(suppl):S133-S143. https://www.ncbi.nlm.nih.gov/pubmed/9894478 [3] Li G, Hansmann ML, Zwingers T, et al. Primary lymphoma of the lung :morphological, immunohistochemical and clinical features[J]. Histopathology, 1990, 16(6):519-531. doi: 10.1111/j.1365-2559.1990.tb01157.x [4] Fiche M, Capron F, Berger F, et al. Primary pulmonary non-Hodg kin's lymphomas[J]. Histopathology, 1995, 26(6):529-537. doi: 10.1111/j.1365-2559.1995.tb00271.x [5] Borie R, Wislez M, Thabut G, et al. Clinical characteristics and prognostic factors of pulmonary MALT lymphoma[J]. Eur Respir J, 2009, 34(6):1408-1416. doi: 10.1183/09031936.00039309 [6] Thieblemont C, Berger F, Dumontet C, et al. Mucosa-associated lymphoid tissue lymphoma is a disseminated disease in one third of 158 patients analyzed[J]. Blood, 2000, 95(3):802-806. doi: 10.1182/blood.V95.3.802.003k19_802_806 [7] Chng WJ, Remstein ED, Fonseca R, et al. Gene expression profiling of pulmonary mucosa-associated lymphoid tissue lymphoma identifies new biologic insights with potential diagnostic and therapeutic applications[J]. Blood, 2009, 113(3):635-645. doi: 10.1182/blood-2008-02-140996 [8] Nicholson AG, Wotherspoon AC, Jones AL, et al. Pulmonary B-cell non-Hodgkin's lymphoma associated with autoimmune disorders: a clinic pathological review of six cases[J]. Eur Respir J, 1996, 9(10):2022-2025. doi: 10.1183/09031936.96.09102022 [9] Oh SY, Kim WS, Kim JS, et al. Pulmonary marginal zone B-celllymphoma of MALT type-What is a prognostic factor and which is the optimal treatment, operation, or chemotherapy?: Consortium for Improving Survival of Lymphoma(CISL) Study[J]. Ann Hematol, 2010, 89(6):563-568. doi: 10.1007/s00277-009-0875-7 [10] Bae YA, Lee KS, Han J, et al. Marginal zone B-cell lymphoma of bronchusassociated lymphoid tissue (BALT): imaging findings in 21 patients[J]. Chest, 2008, 133(2):433-440. doi: 10.1378/chest.07-1956 [11] Maksimovie O, Bethge WA, Pintoffl JP, et al. Marginal zone B-cell non-Hodgkin's lymphoma of musco-associated lymphoid tissue type:imaging findings[J]. AJR Am J Roentgenol, 2008, 191(3): 921-930. doi: 10.2214/AJR.07.2629 [12] Imai H, Sunaga N, Kaira K, et al. Clinicopathological features of patients with bronchial-associated lymphoid tissue lymphoma[J]. Int Med, 2009, 48(5):301-306. https://www.academia.edu/19347002/Clinicopathological_Features_of_Patients_with_Bronchial-Associated_Lymphoid_Tissue_Lymphoma [13] Harris NL, Isaacson PG. What are the criteria for distinguishing MALT from non-MALT lymphoma at extranodal sites[J]? Am J Cli Pathol, 1999, 111(1 Suppl 1):126-132. http://europepmc.org/abstract/MED/9894477 [14] Stefanovic A, Morgensztern D, Fong T, et al. Pulmonary marginal zone lymphoma: a single centre experience and review of the SEER database[J]. Leuk Lymphoma, 2008, 49(7):1311-1320. doi: 10.1080/10428190802064933 -




 下载:
下载: