Prognostic value of the number of negative lymph nodes in non-small cell lung cancer without lymphatic metastasis after pulmonary resection
-
摘要:
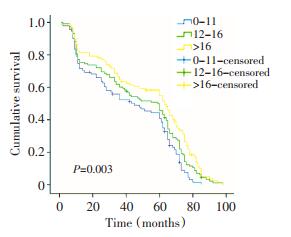
目的 探讨淋巴结清扫数目对无淋巴结转移非小细胞肺癌患者预后的影响。 方法 回顾性分析305例无淋巴结转移非小细胞肺癌患者临床病理资料。 结果 全组患者中位生存期和5年生存率分别为60.0个月和47.1%。T分期、淋巴结清扫数目和清扫站数是影响本组患者预后的独立预后因素。相同T分期患者生存率随淋巴结清扫数目增加而增高(P < 0.05)。T1~T2的患者中,清扫0~11枚淋巴结的患者比清扫更多数目的各组患者预后差(P <0.05)。T3的患者中,清扫0~16枚淋巴结的患者比清扫更多数目的患者预后差(P <0.05)。淋巴结清扫数目与术后并发症发生率无显著相关性(P>0.05)。 结论 淋巴结清扫数目是无淋巴结转移非小细胞肺癌患者预后的独立预后因素。术中应清扫足够数目的淋巴结,进而提高患者生存率。 Abstract:Objective This study aims to investigate the correlation between the number of resected lymph nodes (LNs) and the prognosis of patients with node-negative non-small cell lung cancer (NSCLC). Methods A retrospective review of 305 patients with NSCLC, who received curative resection between January 2004 and December 2009, was conducted. All patients were proved without lymph node involvement histopathologically. The prognostic impact of the number of negative LNs and the clinicopathologic factors were analyzed. Results The overall median survival time and the 1-, 3-, and 5-year overall survival rates were 60.0 months, 76.1%, 59.3%, and 47.1%, respectively. Survival analysis confirmed that the number of negative LNs, T staging and the stations of the mediastinal lymph nodes dissected were showed to be independent prognostic factors. Patients with a high number of negative LNs had better overall survival than patients with a low number of negative LNs (P <0.05). The patients with dissected LNs counts of more than 11 for cases with pTl~2 tumor (P <0.05) and more than 16 for cases with pT3 tumor (P <0.05) had better long-term survival outcomes. The post-operative complication rate was 12.1%, which was not significantly correlated with the number of dissected lymph nodes (P>0.05). Conclusion The number of negative lymph nodes is an independent prognostic predicting factor for node-negative NSCLC. Sufficient dissection of LNs is recommended to improve the survival of the patients with node-negative NSCLC. -
Key words:
- non-small cell lung cancer /
- lymph nodes /
- lymphadenectomy /
- prognosis
-
表 1 不同淋巴结清扫数目患者中位生存期及1、3、5年生存率
Table 1. Survival rate and median survival time of patients according to their different numbers of lymph nodes dissection

表 2 影响患者预后的临床病理因素单因素分析
Table 2. Univariate analysis for the prognosis of 305 patients with pT1-3N0M0

表 3 影响患者预后的Cox比例风险模型分析
Table 3. Cox regression analysis of prognostic factors influencing the overall survival

表 4 不同T分期中淋巴结清扫数目切点的生存率差异
Table 4. Survival rate of the different T staging patients according to the different numbers of lymph nodes dissection

表 5 淋巴结清扫数目与术后并发症发生率Logistic回归分析
Table 5. Logistic regression analysis of the number of lymph nodes dissection and post-operative complication rate

-
[1] Le Chevalier T. Adjuvant chemotherapy for resectable non-small-cell lung cancer: where is it going[J]? Ann Oncol, 2010, 21(Suppl 7): 196-198. http://cn.bing.com/academic/profile?id=7a0836587c78b29babc7037fb299f77b&encoded=0&v=paper_preview&mkt=zh-cn [2] Groome PA, Bolejack V, Crowley JJ, et al. The IASLC Lung Cancer Staging Project: validation of the proposals for revision of the T, N, and M descriptors and consequent stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours[J]. J Thorac Oncol, 2007, 2(8):694-705. doi: 10.1097/JTO.0b013e31812d05d5 [3] Huang CM, Lin JX, Zheng CH, et al. Effect of negative lymph node count on survival for gastric cancer after curative distal gastrectomy[J]. Eur J Surg Oncol, 2011, 37(6):481-487. doi: 10.1016/j.ejso.2011.01.012 [4] 王腾, 华东, 郁皓.阴性淋巴结数目预测胃癌术后生存的临床价值[J].中国肿瘤临床, 2010, 37(2):101-103.Wang T, Hua D, Yu H. Association of the Number of Negative Lymph Nodes with Prognosis of Post-operative Gastric Cancer Patients[J]. Chin J Clin Oncol, 2010, 37(2):101-103. [5] Hsu PK, Huang CS, Wang BY, et al. The prognostic value of the number of negative lymph nodes in esophageal cancer patients after transthoracic resection[J]. Ann Thorac Surg, 2013, 96(3):995-1001. doi: 10.1016/j.athoracsur.2013.04.098 [6] Takenaka T, Katsura M, Shikada Y, et al. Outcome of surgical resection as a first line therapy in T3 non-small cell lung cancer patients[J]. World J Surg, 2013, 37(11):2574-2580. doi: 10.1007/s00268-013-2174-7 [7] Donington J, Ferguson M, Mazzone P, et al. American College of Chest Physicians and Society of Thoracic Surgeons consensus statement for evaluation and management for high-risk patients with stage Ⅰ non-small cell lung cancer[J]. Chest, 2012, 142(6):1620-1635. doi: 10.1378/chest.12-0790 [8] Cerfolio RJ, Bryant AS, Minnich DJ. Complete thoracic mediastinal lymphadenectomy leads to a higher rate of pathologically proven N2 disease in patients with non-small cell lung cancer[J]. Ann Thorac Surg, 2012, 94(3):902-906. doi: 10.1016/j.athoracsur.2012.05.034 [9] Gajra A, Newman N, Gamble GP, et al. Effect of number of lymph nodes sampled on outcome in patients with stage Ⅰ non-small-cell lung cancer[J]. J Clin Oncol, 2003, 21(6):1029-1034. doi: 10.1200/JCO.2003.07.010 [10] Wu YC, Lin CF, Hsu WH, et al. Long-term results of pathological stage Ⅰ non-small cell lung cancer: validation of using the number of totally removed lymph nodes as a staging control[J]. Eur J Cardiothorac Surg, 2003, 24(6):994-1001. doi: 10.1016/S1010-7940(03)00567-0 [11] Li SH, Wang Z, Liu XY, et al. Gene diagnosis and prognostic significance of lymph node micrometastasis after complete resection of histologically node-negative non-small cell lung cancer[J]. World J Surg, 2008, 32(8):1651-1656. doi: 10.1007/s00268-008-9560-6 [12] Lardinois D, De Leyn P, Van Schil P, et al. ESTS guidelines for intraoperative lymph node staging in non-small cell lung cancer[J]. Eur J Cardiothorac Surg, 2006, 30(5):787-792. doi: 10.1016/j.ejcts.2006.08.008 [13] Allen JW, Farooq A, O'Brien TF, et al. Quality of surgical resection for nonsmall cell lung cancer in a US metropolitan area[J]. Cancer, 2011, 117(1):134-142. http://cn.bing.com/academic/profile?id=8029ed1e92a727c9f0b797c006f15d30&encoded=0&v=paper_preview&mkt=zh-cn [14] Verhagen AF, Schoenmakers MC, Barendregt W, et al. Completeness of lung cancer surgery: is mediastinal dissection common practice[J]? Eur J Cardiothorac Surg, 2012, 41(4):834-838. http://cn.bing.com/academic/profile?id=5f2ab58bcbb0a9ac96c3e7fa91f96699&encoded=0&v=paper_preview&mkt=zh-cn [15] 董博鸣, 张林, 张文涛, 等.肺癌纵隔淋巴结廓清术与术后并发症关系的探讨[J].中华胸心血管外科杂志, 2004, 20(1):57-58. doi: 10.3760/cma.j.issn.1001-4497.2004.01.031Dong BM, Zhang L, Zhang WT, et al. The relation of postoperative complications and mediastinal lymph node dissection in lung cancer[J]. Chin J Thorac Cardiovasc Surg, 2004, 20(1):57-58. doi: 10.3760/cma.j.issn.1001-4497.2004.01.031 [16] Sugi K, Nawata K, Fujita N, et al. Systematic lymph node dissection for clinically diagnosed peripheral non-small-cell lung cancer less than 2 cm in diameter[J]. World J Surg, 1998, 22(3):290-295. doi: 10.1007/s002689900384 [17] Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial[J]. J Thorac Cardiovasc Surg, 2011, 141(3):662-670. doi: 10.1016/j.jtcvs.2010.11.008 [18] Howington JA, Blum MG, Chang AC, et al. Treatment of stage Ⅰ and Ⅱ non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines[J]. Chest, 2013, 143(5 Suppl):e278S-e313S. doi: 10.1378/chest.12-2359 -




 下载:
下载: