Clinicopathological characteristics of axillary lymph node metastasis in lung cancer
-
摘要:
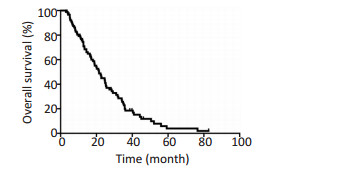
目的 总结肺癌伴腋窝淋巴结转移(axillary lymph node metastasis,ALNM)的临床特点。 方法 回顾性分析2007年1月至2013年12月浙江省肿瘤医院收治的91例肺癌ALNM的患者资料。采用列联表分析原发灶、颈部和锁骨上区淋巴结、纵隔淋巴结与腋窝淋巴结位置相关性,采用Kaplan-Meier法计算总生存,以及不同时期发现ALNM患者的生存情况,并行Log-rank检验,进一步进行Cox回归分析。 结果 肺癌伴ALNM发生率为0.63%;常见于腺癌患者,以周围型病灶多见,常累及胸膜并伴胸水,或发生胸壁转移。原发灶、颈部和锁骨上区淋巴结、纵隔淋巴结与腋窝淋巴结位置存在相关性。肺癌伴ALNM的患者中位生存时间为19.02个月,2年生存率为62.64%。首诊伴ALNM患者生存情况差于首诊无腋窝淋巴结患者,且为独立预后因子(P=0.003,RR=2.18,95%CI:1.330~3.572)。 结论 肺癌伴ALNM发生率低,其可能的转移途径为胸壁、淋巴引流及血行转移,首诊发现ALNM的患者生存情况更差。 Abstract:Objective To investigate the clinicopathological characteristics of lung cancer patients with axillary lymph node metastasis (ALNM). Methods The clinical data of 91 lung cancer patients with ALNM who were treated in Zhejiang Cancer Hospital from January 1st, 2007 to December 31st, 2013 were retrospectively analyzed. The relevance of the sites of the tumor site, local lymph node, and axillary lymph node was checked by contingency table. Survival rates were calculated by the Kaplan-Meier method and compared by a log-rank test. Cox proportional hazards model was applied to analyze the prognostic factors. Results The proportion of lung cancer patients with ALNM was 0.63%, and the patients were often presented with adenocarcinoma, peripheral tumor type, pleura invasion with pleural effusion, or chest wall invasion. A relationship between tumor sites, local lymph node sites, and axillary lymph node sites was observed. The median survival time of lung cancer patients with ALNM was 19.02 months, and the two-year survival rate is 62.64%. Patients identified with ALNM at the initial diagnosis reported poor prognosis (P=0.002). Cox regression analysis showed that the relative risk of death in patients with ALNM at initial diagnosis was elevated 2.18 times (95%CI: 1.330-3.572, P=0.003). Conclusion ALNM in lung cancer is rare, and it may involve through direct chest wall invasion and spread from supraclavicular and mediastinal lymph node metastasis or systemic origin. Patients detected with ALNM at the initial diagnosis indicated poor prognosis. -
表 1 91例肺癌伴ALNM患者临床资料
Table 1. Clinical data of 91 lung cancer patients with ALNM

表 2 91例肺癌患者ALNM特点
Table 2. Clinical data of ALNM of 91 lung cancer patients

表 3 86例肺癌伴ALNM患者复发转移情况
Table 3. Recurrence and metastasis of 86 lung cancer patients with ALNM

表 4 原发灶、锁上颈部淋巴结、纵隔淋巴结与腋窝淋巴结位置相关性
Table 4. Relevance of primary tumor and lymph node position

-
[1] Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015 [J]. CA Cancer J Clin, 2016, 66(2):115-132. doi: 10.3322/caac.21338 [2] Marc Riquet FoLP-B, Claire Danel. Axillary lymph node metastases from bronchogenic carcinoma[J]. Ann Thorac Surg, 1998, 6(6):920-923. doi: 10.1002/1097-0142(19950901)76:5%3C803::AID-CNCR2820760514%3E3.0.CO;2-0/abstract [3] Fishman EK, Zinreich ES, Jacobs CG, et al. CT of the axilla normal anatomy and pathology[J]. Radio Graphics, 1986, 6(3):475-502. http://www.docin.com/p-1623928652.html [4] Kamiyoshihara M, Kawashima O, Ishikawa S, et al. Mediastinal lymph node evaluation by computed tomographic scan in lung cancer[J]. J Cardiovasc Surg (Torino), 2001, 42(1):119-124. https://www.researchgate.net/publication/12040977_Mediastinal_lymph_node_evaluation_by_computed_tomographic_scan_in_lung_cancer [5] David R. Marcantonio HIL. Axillary lymph node metastases of bronchogenic carcinoma[J]. Cancer, 1995, 76(5):803-806. doi: 10.1002/(ISSN)1097-0142 [6] Satoh H, Ishikawa H, Kagohashi K, et al. Axillary lymph node metastasis in lung cancer[J]. Med Oncol, 2009, 26(2):147-150. doi: 10.1007/s12032-008-9097-4 [7] Kim AW. Lymph node drainage patterns and micrometastasis in lung cancer[J]. Semin Thorac Cardiovasc Surg, 2009, 21(4):298-308. doi: 10.1053/j.semtcvs.2009.11.001 [8] 李鉴, 张德超, 赫捷, 等.肺腺鳞癌淋巴结转移规律的探讨[J].中华肿瘤杂志, 2009, 31(7):524-527. http://www.cqvip.com/QK/93685X/200907/31145479.htmlLi J, Zhang DC, He J, et al. The rule of lymph node metastasis of adenosquamous carcinoma of the lung[J]. Chin J Oncol, 2009, 31(7): 524-527. http://www.cqvip.com/QK/93685X/200907/31145479.html -




 下载:
下载: