Effects of ropivacaine as intercostal nerve blocker on postoperative pain after video-assisted thoracic surgery of lung cancer patients
-
摘要:
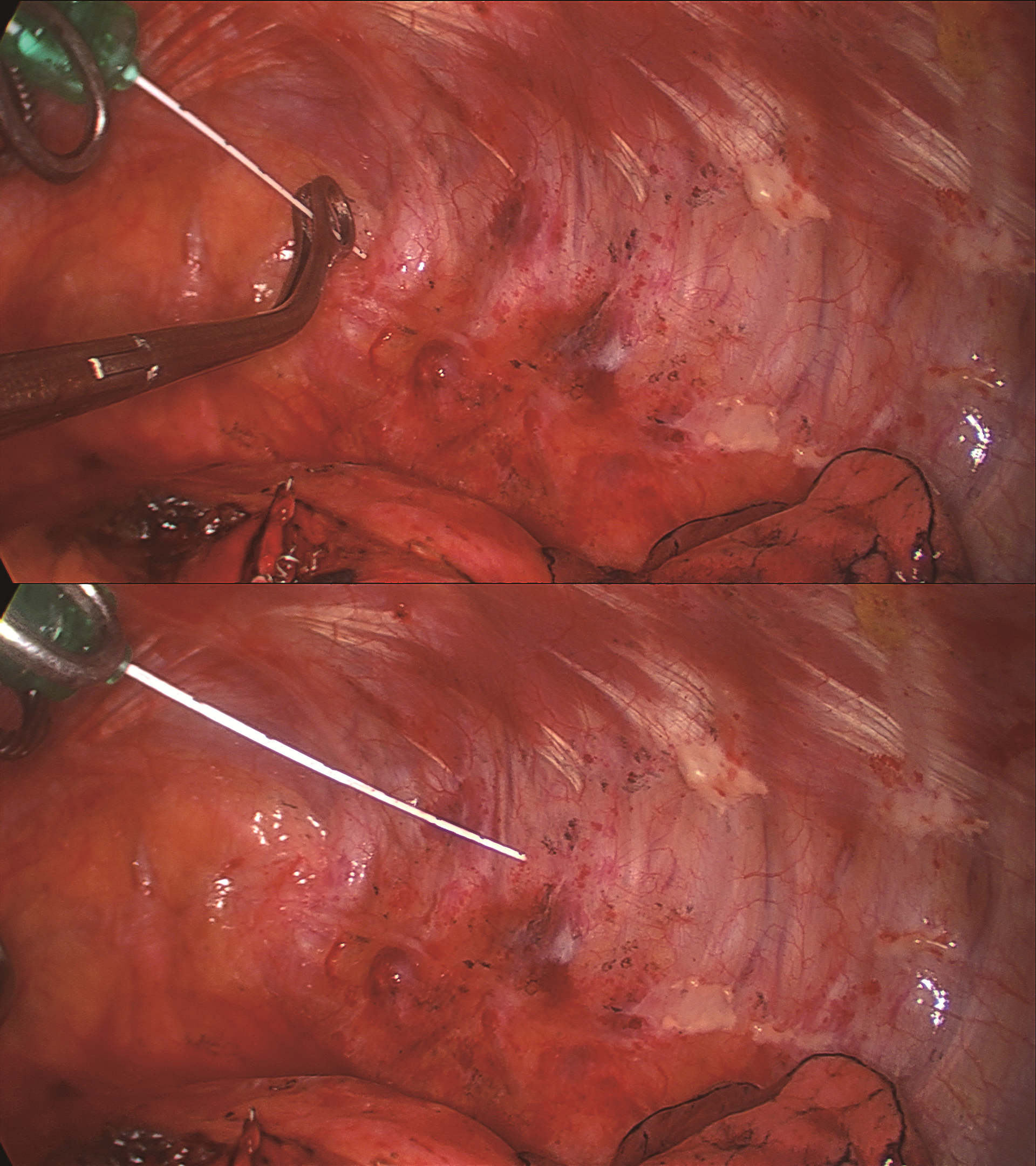
目的 探讨罗哌卡因肋间神经阻滞对肺癌患者胸腔镜术后镇痛效果的影响。 方法 分析2016年10月至2016年12月天津医科大学肿瘤医院60例接受肺癌胸腔镜手术治疗的患者,男性35例,女性25例,随机分为2组,分别为0.25%罗哌卡因阻滞组(试验组)和对照组,关胸前行肋间神经阻滞,每一肋间给药3 mL,拔出气管插管后行PCIA镇痛。记录拔管后12 h(T1)、24 h(T2)、48 h(T3)、72 h(T4)时试验组及对照组静息时疼痛VAS评分及Prince-Henry(P-H)评分;以及术后吗啡追加剂量和不良反应事件。 结果 试验组术后T1~T4各时间点VAS和P-H评分均低于对照组(P<0.01)。术后试验组咳嗽费力、肺部感染、肺不张等呼吸系统并发症发生率较低(P<0.05)。 结论 罗哌卡因肋间神经阻滞可有效减轻肺癌术后患者疼痛并降低术后呼吸系统并发症。 Abstract:Objective To investigate the effects of ropivacaine as intercostal nerve blocker on postoperative pain after video-assistedthoracic surgery(VATS)of lung were cancer patients. Methods A total of 60 patients who underwent elective VATS were randomly divided into two groups.The patients in control group were ereated with intercostal nerve blocker with saline.The patients in test groupwere administrated with intercostal nerve blocker with 0.25% ropivacaine.The effects were evaluated using the visual analogue scale(VAS)and Prince Henry Pain Scale(PHPS)at 12(T1), 24(T2), 48(T3), and 72 h(T4) after extubation.Moreover, the adverse events anddosage of morphine after surgery were measured. Results Compared with the control group, the VAS and PHPS scores of the testgroup were significantly low at T1-T4(P < 0.01).Postoperative respiratory complications, such as pulmonary infection and atelectasis, were less in the test group(P < 0.05) than control. Conclusion Intercostal nerve block with ropivacaine provides good analgesic effectsfor patients underwent VATS. -
Key words:
- ropivacaine /
- intercostal nerve block /
- lung cancer /
- analgesia
-
表 1 患者不同时间点VAS评分及PHPS评分的比较
Table 1. Comparison of VAS and PHPS scales between the test and control groups

表 2 患者术后带管时间及吗啡用量的比较
Table 2. Comparison of the dosage of morphine and the time of intubation between test group and control group

表 3 患者术后咳嗽及感染情况的比较
Table 3. Comparison of cough and infection in test and control group

-
[1] 中华医学会麻醉学分会.成人术后疼痛处理专家共识[J].临床麻醉学杂志, 2010, 26(3):7. http://www.cnki.com.cn/Article/CJFDTOTAL-LCMZ201003003.htmThe Chinese Medical Association Branch of Anesthesiology. Expert consensus on postoperative pain management in adults[J]. J ClinAnesthesiol, 2010, 26(3):7. http://www.cnki.com.cn/Article/CJFDTOTAL-LCMZ201003003.htm [2] Merskey H. Logic, truth and language in concepts of pain[J]. Qual Life Res, 1994, 3(Suppl 1):S69-76. https://www.ncbi.nlm.nih.gov/pubmed/7866375 [3] Bardiau FM, Taviaux NF, Albert A, et al. An intervention study to enhance postoperative pain management[J]. Anesth Analg, 2003, 96(1):179-185. http://cat.inist.fr/?aModele=afficheN&cpsidt=14467784 [4] 刘飞, 张静, 张欢楷, 等.超声引导胸椎旁阻滞治疗胸腔镜手术后早期中重度急性疼痛的疗效观察[J].中华医学杂志, 2017, 92(02):119-122. doi: 10.3760/cma.j.issn.0376-2491.2017.02.008Liu F, Zhang J, Zhang HK, et al. Thoracic paravertebral block in the PACU for immediate postoperative pain relief after video-assisted thoracoscopic surgery[J]. Natl Med J China, 2017, 97(2):119-122. doi: 10.3760/cma.j.issn.0376-2491.2017.02.008 [5] Fibla JJ, Molins L, Mier JM, et al. The efficacy of paravertebral block using a catheter technique for postoperative analgesia in thoracoscopic surgery: a randomized trial[J]. Eur J Cardiothorac Surg, 2011, 40(4):907-911. http://ejcts.oxfordjournals.org/content/40/4/907.long [6] Guay J. The benefits of adding epidural analgesia to general anesthesia: a metaanalysis[J]. J Anesth, 2006, 20(4):335-340. doi: 10.1007/s00540-006-0423-8 [7] Rodgers A, Walker N, Schug S, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials[J]. BMJ, 2000, 321(7275):1493. doi: 10.1136/bmj.321.7275.1493 [8] Ochroch EA, Gottschalk A. Impact of acute pain and its management for thoracic surgical patients[J]. Thorac Surg Clin, 2005, 15(1):105-121. doi: 10.1016/j.thorsurg.2004.08.004 [9] Vogt A, Stieger DS, Theurillat C, et al. Single-injection thoracic paravertebral block for postoperative pain treatment after thoracoscopic surgery[J]. Br J Anaesth, 2005, 95(6):816-821. doi: 10.1093/bja/aei250 [10] Ishikawa Y, Maehara T, Nishii T, et al. Intrapleural analgesia using ropivacaine for postoperative pain relief after minimally invasive thoracoscopic surgery[J]. Ann Thorac Cardiovasc Surg, 2012, 18(5):429-433. doi: 10.5761/atcs.oa.11.01854 [11] D'Andrilli A, Ibrahim M, Ciccone AM, et al. Intrapleural intercostal nerve block associated with mini-thoracotomy improves pain control after major lung resection[J]. Eur J Cardiothorac Surg, 2006, 29(5):790-794. doi: 10.1016/j.ejcts.2006.01.002 -




 下载:
下载: