Prognostic value of pretreatment platelet and fibrinogen levels for early non-small cell lung cancer after complete resection
-
摘要:
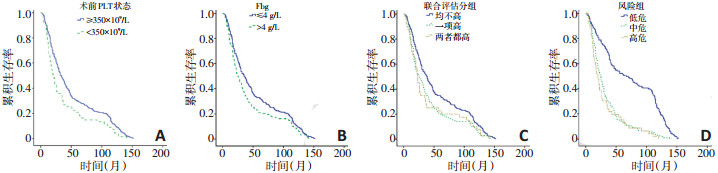
目的 评估血小板及纤维蛋白原对于根治术后非小细胞肺癌的预后价值,并建立预后模型以早期发现术后预后较差的患者。 方法 选取2004年3月至2009年1月在天津医科大学肿瘤医院行根治性手术且术后病理确诊的非小细胞肺癌患者405例,血小板及纤维蛋白原水平均为术前测定,并对相关临床病理指标及生存期进行分析。 结果 血小板和纤维蛋白原水平升高的发生率分别为16.5%和36.3%。血小板和/或纤维蛋白原升高的患者生存期较短。多因素分析提示病理分期(P<0.05)、复发或转移(P<0.05)及血小板水平(P<0.05)为非小细胞肺癌的独立预后因素。低危组、中危组及高危组患者的中位生存期分别为67、24和20个月,有显著性差异(P<0.05)。 结论 术前血小板及血浆纤维蛋白原与非小细胞肺癌患者的预后有密切关系,风险模型的建立或可较早发现高危患者并尽早给予个体化治疗从而改善预后。 Abstract:Objective To evaluate the prognostic value of pretreatment platelet and fibrinogen levels for non-small cell lung cancer (NSCLC) after complete resection. Methods Four hundred and five patients with pathological-proven NSCLC who underwent complete resection between March 2004 and January 2007 were included in this study. Blood samples for pretreatment platelet and fibrinogen examinations were collected. Platelet and fibrinogen levels were analyzed with patients' clinical parameters. Results The overall prevalence of thrombocytosis (>350×109/L) was 16.5%, and that of hyperfibrinogenemia (>4 g/L) was 36.3%. Patients with thrombocytosis and/or hyperfibrinogenemia exhibited poor overall survival (P=0.002). Multivariate survival analysis using the Cox proportional hazard model demonstrated that pretreatment platelet levels (P=0.048), tumor stage (P < 0.05), and tumor progression (P < 0.05) were independent prognostic factors of NSCLC. The median survival time among patients with low-, intermediate-, and high-risk NSCLC were 67, 24, and 20 months, respectively (P < 0.05). Conclusions Elevated pretreatment platelet and fibrinogen levels significantly correlate with poor survival in patients with NSCLC. Moreover, the risk model can potentially improve prognosis by enabling the detection of highrisk patients and providing a reference for individualized treatments. -
Key words:
- platelets /
- fibrinogen /
- prognosis /
- neoplasm metastasis /
- non-small-cell lung cancer
-
表 1 非小细胞肺癌患者术前的血小板及纤维蛋白原水平(中位数)

表 2 非小细胞肺癌预后的单因素分析(Kaplan-Meier法)

表 3 多因素分析Cox比例风险回归模型

表 4 联合血小板及纤维蛋白原预测复发转移及预后

-
[1] Siegel RL, Miller KD, Jemal A.Cancer Statistics 2017[J]. CA Cancer J Clin, 2017, 67(1):7-30. doi: 10.3322/caac.21387 [2] Zheng, R, Zeng, H, Zuo, T, et al. Lung cancer incidence and mortality in China 2011[J]. Thorac Cancer, 2016, 7(1):94-99. doi: 10.1111/1759-7714.12286 [3] Møller Pedersen, L. Milman N. Prognostic significance of thrombocytosis in patients with primary lung cancer[J]. Eur Respir J, 1996, 9(9): 1826-1830. doi: 10.1183/09031936.96.09091826 [4] Ikeda M, Furukawa H, Imamura H, et al.Poor prognosis associated with thrombocytosis in patients with gastric cancer[J]. Ann Surg Oncol, 2002, 9(3):287-291. doi: 10.1007/BF02573067 [5] Hwang SG, Kim KM, Cheong JH, et al. Impact of pretreatment thrombocytosis on blood-borne metastasis and prognosis of gastric cancer[J]. Eur J Surg Oncol, 2012, 38(7):562-567. doi: 10.1016/j.ejso.2012.04.009 [6] Perisanidis C, Psyrri A, Cohen EE. et al. Prognostic role of pretreatment plasma fibrinogen in patients with solid tumors: A systematic review and meta-analysis[J]. Cancer Treat Rev, 2015, 41(10):960-970. doi: 10.1016/j.ctrv.2015.10.002 [7] Hernandez E, Donohue KA, Anderson LL, et al. The significance of thrombocytosis in patients with locally advanced cervical carcinoma: a Gynecologic Oncology Group study[J]. Gynecol Oncol, 2000, 78(2):137-142. doi: 10.1006/gyno.2000.5838 [8] Gucer F, Moser F, Tamussino K, et al. Thrombocytosis as a prognostic factor in endometrial carcinoma[J]. Gynecol Oncol, 1998, 70(2): 210-214. doi: 10.1006/gyno.1998.5078 [9] Falanga A, Russo L, Milesi V, et al. Mechanisms and risk factors of thrombosis in cancer[J]. Crit Rev Oncol Hematol, 2017, (118):79-83. https://www.sciencedirect.com/science/article/pii/S1040842817303141 [10] Stegner DS, Dutting B. Nieswandt, Mechanistic explanation for platelet contribution to cancer metastasis[J]. Thromb Res, 2014, 133 Suppl 2: S149-157. http://europepmc.org/abstract/med/24862136 [11] Palumbo JS, Talmage KE, Massari JV, et al. Platelets and fibrin (ogen) increase metastatic potential by impeding natural killer cellmediated elimination of tumor cells[J]. Blood, 2005, 105(1):178-185. doi: 10.1182/blood-2004-06-2272 [12] Martino MM, Briquez PS, Ranga, A, et al. Heparin-binding domain of fibrin(ogen) binds growth factors and promotes tissue repair when incorporated within a synthetic matrix[J]. Proc Natl Acad Sci U S A, 2013, 110(12):4563-4568. doi: 10.1073/pnas.1221602110 [13] Witsch E, Sela M, Yarden Y. Roles for growth factors in cancer progression[J]. Physiology (Bethesda), 2010, 25(2):85-101. http://europepmc.org/articles/PMC3062054 [14] Desgrosellier JS. Cheresh DA. Integrins in cancer: biological implications and therapeutic opportunities[J]. Nat Rev Cancer, 2010, 10(1): p.9-22. doi: 10.1038/nrc2748 [15] Zheng S, Shen J, Jiao Y, et al, Platelets and fibrinogen facilitate each other in protecting tumor cells from natural killer cytotoxicity[J]. Cancer Sci, 2009, 100(5):859-865. doi: 10.1111/j.1349-7006.2009.01115.x [16] Palumbo JS, Kombrinck KW, Drew AF. et al. Fibrinogen is an important determinant of the metastatic potential of circulating tumor cells[J]. Blood, 2000, 96(10):3302-3309. http://europepmc.org/abstract/med/11071621 [17] Ma S, Shen L, Qian N, et al. The prognostic values of CA125, CA19.9, NSE, AND SCC for stage I NSCLC are limited[J]. Cancer Biomark, 2011, 10(3-4):155-162. https://content.iospress.com/articles/cancer-biomarkers/cbm00246 [18] Castelli R, Porro F, Tarsia P. The heparins and cancer: review of clinical trials and biological properties[J]. Vasc Med, 2004, 9(3):205-213. doi: 10.1191/1358863x04vm566ra [19] Cosgrove RH, Zacharski LR, Racine E, et al. Improved cancer mortality with low-molecular-weight heparin treatment: a review of the evidence[J]. Semin Thromb Hemost, 2002, 28(1):79-87. doi: 10.1055/s-2002-20566 [20] Hirschfield G.Effects of fluvastatin and bezafibrate combination on plasma fibrinogen, t-plasminogen activator inhibitor and C reactive protein levels in coronary artery disease patients with mixed hyperlipidaemia (FACT Study)--a rebuttal[J]. Thromb Haemost, 2001, 85 (1):189-190. doi: 10.1055/s-0037-1612931 -




 下载:
下载: