Clinical value of standardized procedures of fine lymph node sorting from gastric cancer samples after curative resection: a study of 727 cases
-
摘要:
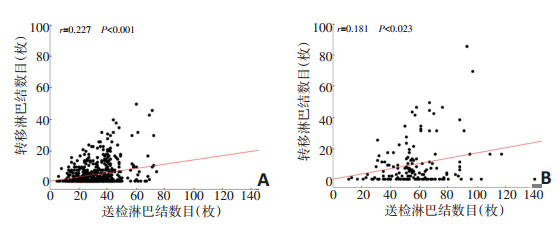
目的 探讨胃癌根治术标本中淋巴结精细分拣的临床应用价值。 方法 回顾性分析2016年1月至2017年12月就诊于天津医科大学肿瘤医院实施胃癌根治术的727例胃癌患者临床病理资料,按照手术切除标本中淋巴结分拣方式分为精细淋巴结分拣组和区域淋巴结分拣组,分析两组患者送检淋巴结数目、转移淋巴结数目的差异并进行相关性分析比较。 结果 两组患者的性别、年龄、肿瘤大小等因素间差异均无统计学意义(P > 0.05),两组之间具有可比性。精细淋巴结分拣组患者淋巴结送检数目明显多于区域淋巴结分拣组(P < 0.001)。在T分期、N分期以及TNM分期相同的情况下,精细淋巴结分拣组送检淋巴结数目显著多于区域淋巴结分拣组(P < 0.001);精细淋巴结分拣组淋巴结转移数目也显著多于区域淋巴结分拣组(P < 0.001)。此外,两组患者送检淋巴结数目与转移淋巴结数目均呈正相关,差异具有统计学意义(精细淋巴结分拣组r=0.181,P=0.023;区域淋巴结分拣组r= 0.227,P < 0.001),且精细淋巴结分拣组患者的送检淋巴结数目与转移淋巴结数目之间相关性弱于区域淋巴结分拣组患者。 结论 胃癌根治术后精细淋巴结分拣可以提高送检淋巴结数目,提供精确的术后淋巴结分期,减少分期迁移,可以在临床上规范性推广。 Abstract:Objective To evaluate the potential clinical value of standardized procedures of fine lymph node sorting from gastric cancer samples after curative resection. Methods Between January 2016 and December 2017, 727 gastric cancer patients who underwent R0 resection in the Tianjin Medical University Cancer Institute and Hospital were retrospectively included and assigned to either the fine lymph node sorting group or regional lymph node sorting group in accordance with the lymph node sorting methods from the tumor samples of all patients. Both the numbers of examined lymph nodes and metastatic lymph nodes were compared between the two groups. Additionally, correlation analyses were performed between the numbers of examined lymph nodes and metastatic lymph nodes in the two groups. Results There was no significant difference in sex, age, or tumor size between the two groups (P > 0.05), indicating that there was comparability between the two groups. The number of examined lymph nodes in the fine lymph node sorting group was significantly higher than that in the regional lymph node sorting group (P < 0.001). Furthermore, the number of examined lymph nodes in the fine lymph node sorting group was much higher than that in the regional lymph node sorting group with the same pT, pN, or pTNM stage (P < 0.001). The number of metastatic lymph nodes in the fine lymph node sorting group was significantly higher than that in the regional lymph node sorting group (P < 0.001). There was a significant positive correlation between the numbers of examined lymph nodes and metastatic lymph nodes in both groups (fine lymph node sorting group r=0.181, P=0.023; regional lymph node sorting group r=0.227, P < 0.001). Additionally, the correlation coefficient between the numbers of examined lymph nodes and metastatic lymph nodes in the fine lymph node sorting group was weaker than that in the regional lymph node sorting group. Conclusions The standard procedures of fine lymph node sorting from tumor samples of gastric cancer may increase the number of examined lymph nodes, accurately provide the postoperative pN stage, reduce the stage migration, and should be applied in clinical standardization. -
Key words:
- gastric cancer /
- lymph node metastasis /
- prognosis
-
表 1 精细淋巴结分拣组和区域淋巴结分拣组患者的临床资料对比 (例)

表 2 精细淋巴结分拣组和区域淋巴结分拣组患者送检淋巴结数目与转移淋巴结数目比较 (枚,x±s)

表 3 pT分期相同时精细淋巴结分拣组和区域淋巴结分拣组患者送检淋巴结数目及转移淋巴结数目比较

表 4 pN分期相同时精细淋巴结分拣组和区域淋巴结分拣组患者送检淋巴结数目及转移淋巴结数目比较

表 5 pTNM分期相同时精细淋巴结分拣组和区域淋巴结分拣组患者送检淋巴结数目比较

-
[1] 邓靖宇, 梁寒.再谈淋巴结转移对胃癌预后评估的意义[J].中华胃肠外科杂志, 2016, 19(2):157-164. doi: 10.3760/cma.j.issn.1671-0274.2016.02.008 [2] In H, Solsky I, Palis B, et al. Validation of the 8th edition of the AJCC TNM Staging system for gastric cancer using the National Cancer Database[J]. Ann Surg Oncol, 2017, 24(12):3683-3691. doi: 10.1245/s10434-017-6078-x [3] 日本胃癌学会.胃癌处理规约[M].东京:金原出版株式会社, 2017. [4] Sano T, Coit DG, Kim HH, et al. Proposal of a new stage grouping of gastric cancer for TNM classification: International Gastric Cancer Association staging project[J]. Gastric Cancer, 2017, 20(2):217-225. doi: 10.1007/s10120-016-0601-9 [5] 邓靖宇, 梁寒.胃癌根治术后规范淋巴结送检的要点及临床意义[J].中华胃肠外科杂志, 2018, 21(10):1183-1190. doi: 10.3760/cma.j.issn.1671-0274.2018.10.020 [6] In H, Ravetch E, Langdon-Embry M, et al. The newly proposed clinical and post-neoadjuvant treatment staging classifications for gastric adenocarcinoma for the American Joint Committee on Cancer (AJCC) staging[J]. Gastric Cancer, 2018, 21(1):1-9. doi: 10.1007/s10120-017-0765-y [7] Schmidt B, Chang KK, Maduekwe UN, et al. D2 lymphadenectomy with surgical ex vivo dissection into node stations for gastric adenocarcinoma can be performed safely in Western patients and ensures optimal staging[J]. Ann Surg Oncol, 2013, 20(9):2991-2999. doi: 10.1245/s10434-013-3019-1 [8] Afaneh C, Levy A, Selby L, et al. Ex Vivo Lymphadenectomy During Gastrectomy for Adenocarcinoma Optimizes Lymph Node Yield[J]. J Gastrointest Surg, 2016, 20(1):165-171. doi: 10.1007/s11605-015-2948-3 [9] Smith DD, Schwarz RR, Schwarz RE. Impact of total lymph node count on staging and survival after gastrectomy for gastric cancer: data from a large US-population database[J]. J Clin Oncol, 2005, 23 (28):7114-7124. doi: 10.1200/JCO.2005.14.621 [10] Son T, Hyung WJ, Lee JH, et al. Clinical implication of an insufficient number of examined lymph nodes after curative resection for gastric cancer[J]. Cancer, 2012, 118(19):4687-4693. doi: 10.1002/cncr.27426 [11] Deng J, Yamashita H, Seto Y, et al. Increasing the number of examined lymph nodes is prerequisite for improvement accurate evaluation the overall survival of node-negative gastric cancer patients[J]. Ann Surg Oncol, 2017, 24(3):745-753. doi: 10.1245/s10434-016-5513-8 [12] Coburn NG, Swallow CJ, Kiss A, et al. Significant regional variation in adequacy of lymph node assessment and survival in gastric cancer [J]. Cancer, 2006, 107(9):2143-2151. doi: 10.1002/(ISSN)1097-0142 [13] 梁寒.局部进展期胃癌的精准淋巴结清扫[J].中华胃肠外科杂志, 2016, 19(2):138-143. doi: 10.3760/cma.j.issn.1671-0274.2016.02.004 [14] Datta J, Lewis RS Jr, Mamtani R, et al. Implications of inadequate lymph node staging in resectable gastric cancer: a contemporary analysis using the National Cancer Data Base[J]. Cancer, 2014, 120 (18):2855-2865. doi: 10.1002/cncr.28780 [15] Manzoni G, Verlato G, Roviello F, et al. The new TNM classification of lymph node metastasis minimises stage migration problems in gastric cancer patients[J]. Br J Cancer, 2002, 87(2):171-174. doi: 10.1038/sj.bjc.6600432 [16] Deng J, Zhang R, Pan Y, et al. Comparison of the staging of regional lymph nodes using the sixth and seventh editions of the tumornode-metastasis (TNM) classification system for the evaluation of overall survival in gastric cancer patients: findings of a case-control analysis involving a single institution in China[J]. Surgery, 2014, 156 (1):64-74. doi: 10.1016/j.surg.2014.03.020 [17] Deng J, Liu J, Wang W, et al. Validation of clinical significance of examined lymph node count for accurate prognostic evaluation of gastric cancer for the eighth edition of the American Joint Committee on Cancer (AJCC) TNM staging system[J]. Chin J Cancer Res, 2018, 30(5): 477-491. doi: 10.21147/j.issn.1000-9604.2018.05.01 [18] Kim CY, Yang DH. Adjustment of N stages of gastric cancer by the ratio between the metastatic and examined lymph nodes[J]. Ann Surg Oncol, 2009, 16(7):1868-1874. doi: 10.1245/s10434-009-0430-8 [19] Deng J, Zhang R, Wu L, et al. Superiority of the ratio between negative and positive lymph nodes for predicting the prognosis for patients with gastric cancer[J]. Ann Surg Oncol, 2015, 22(4):1258- 1266. doi: 10.1245/s10434-014-4121-8 [20] Sun Z, Xu Y, Li de M, et al. Log odds of positive lymph nodes: a novel prognostic indicator superior to the number-based and the ratiobased N category for gastric cancer patients with R0 resection[J]. Cancer, 2010, 116(11):2571-2580. doi: 10.1002/cncr.v116:11 [21] Kong SH, Lee HJ, Ahn HS, et al. Stage migration effect on survival in gastric cancer surgery with extended lymphadenectomy: the reappraisal of positive lymph node ratio as a proper N-staging[J]. Ann Surg, 2012, 255(1):50-58. doi: 10.1097/SLA.0b013e31821d4d75 [22] Deng J, Liang H. Discussion of the applicability of positive lymph node ratio as a proper N-staging for predication the prognosis of gastric cancer after curative surgery plus extended lymphadenectomy[J]. Ann Surg, 2012, 256(6):e35-36. doi: 10.1097/SLA.0b013e3182769545 [23] Rosa F, Tortorelli AP, Alfieri S, et al. Lymph node ratio for gastric cancer: useful instrument or just an expedient to retrieve fewer lymph nodes[J]? Ann Surg, 2014, 259(4):e65. doi: 10.1097/SLA.0000000000000316 -




 下载:
下载: