Effect of the preoperative Geriatric Nutritional Risk Index on the prognosis of patients with esophageal squamous cell carcinoma after radical resection
-
摘要:
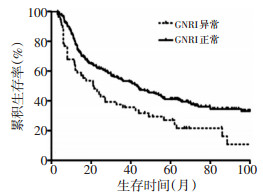
目的 探讨术前老年营养风险指数(Geriatric Nutritional Risk Index,GNRI)对食管鳞癌患者根治性切除术后预后的评估价值。 方法 回顾性分析天津医科大学肿瘤医院2008年1月至2012年12月行根治性手术切除的315例年龄>60岁食管鳞癌患者的临床病理学及实验室资料。GNRI=1.489×血清白蛋白(g/L)+41.7×(体重/理想体重)。根据GNRI水平将患者分为GNRI正常组和GNRI异常组,χ2检验分析GNRI与患者临床病理特征之间的关系,采用Kaplan-Meier法进行生存分析,生存率比较采用Log-rank检验,Cox比例风险回归模型进行多因素生存分析。 结果 GNRI正常组(GNRI>98)259例,GNRI异常组(GNRI≤98)56例。GNRI与患者年龄、肿瘤部位、肿瘤直径、血清白蛋白水平、BMI和淋巴结转移密切相关(均P < 0.05)。GNRI正常组与异常组患者的5年生存率分别为41.2%和27.0%,差异具有统计学意义(P=0.002)。单因素分析显示:年龄、肿瘤直径、血清白蛋白水平、BMI、GNRI、PLR、肿瘤浸润深度和淋巴结转移是影响食管鳞癌患者预后的危险因素(均P < 0.05);多因素分析结果显示,术前GNRI(HR= 0.687,95%CI:0.487~0.968,P=0.032)异常是影响食管鳞癌患者预后的独立危险因素。亚组分析显示,无论有无淋巴结转移,GNRI正常组患者的生存均显著高于GNRI异常组患者(P=0.036和0.010)。 结论 术前GNRI与老年食管鳞癌患者恶性生物学行为相关,可作为预测患者根治术后生存的有用指标。 Abstract:Objective To evaluate the prognostic value of the preoperative Geriatric Nutritional Risk Index (GNRI) in patients with esophageal squamous cell carcinoma after radical resection. Methods Clinicopathological and laboratory data of 315 elderly patients with esophageal squamous cell carcinoma who were older than 60 years and underwent radical resection in Tianjin Medical University Cancer Institute and Hospital from January 2008 to December 2012 were retrospectively analyzed. The GNRI formula was as follows: 1.489 × serum albumin (g/L) + 41.7 × (current body weight/ideal body weight). According to the GNRI, patients were divided into the normal and abnormal GNRI groups. The χ2 test was used to analyze the relationship between the GNRI and the clinicopathological characteristics of patients. The Kaplan-Meier method was used to analyze the survival rate, and survival analysis was conducted using the Log-rank test. Multivariate survival analysis was conducted using the Cox proportional risk regression model. Results There were 259 patients in the normal GNRI group (GNRI>98) and 56 patients in the abnormal GNRI group (GNRI≤98). The GNRI was closely correlated with age, tumor location, tumor diameter, serum albumin level, body mass index (BMI), and lymph node metastasis (all P < 0.05). The 5- year survival rates in the normal and abnormal GNRI groups were 41.2% and 27.0%, respectively, with statistical significance (P=0.002). Univariate analysis showed that age, tumor diameter, serum albumin level, BMI, GNRI, platelet- lymphocyte ratio, tumor invasion depth, and lymph node metastasis were risk factors for the prognosis of patients with esophageal squamous cell carcinoma (all P < 0.05). Multivariate analysis showed that the preoperative GNRI (hazard ratio=0.687, 95% confidence interval: 0.487-0.968, P=0.032) was an independent factor affecting the prognosis of patients with esophageal squamous cell carcinoma. Subgroup analysis showed that the survival rates in the normal GNRI group were significantly higher than those in the abnormal GNRI group (P=0.036 and 0.010, respectively), regardless of lymph node metastasis. Conclusions The preoperative GNRI is associated with malignant biological behavior in elderly patients with esophageal squamous cell carcinoma and can be used as a useful indicator for predicting survival after radical resection. -
表 1 术前GNRI与食管鳞癌患者临床病理特征的相关性 n(%)

表 2 影响本组315例食管鳞癌患者预后的单因素分析结果

表 3 影响本组315例食管鳞癌患者预后的多因素分析结果

-
[1] Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population- based registries in 71 countries[J]. Lancet, 2018, 391 (10125):1023-1075. doi: 10.1016/S0140-6736(17)33326-3 [2] Kang M, Chang CT, Sung HH, et al. Prognostic significance of pre- to postoperative dynamics of the prognostic nutritional index for patients with renal cell carcinoma who underwent radical nephrectomy[J]. Ann Surg Oncol, 2017, 24(13):4067-4075. doi: 10.1245/s10434-017-6065-2 [3] Ramos R, Nadal E, Peiro I, et al. Preoperative nutritional status assessment predicts postoperative outcomes in patients with surgically resected non-small cell lung cancer[J]. Eur J Surg Oncol, 2018, 44(9):1419-1424. doi: 10.1016/j.ejso.2018.03.026 [4] Bo Y, Yao M, Zhang L, et al. Preoperative nutritional risk index to predict postoperative survival time in primary liver cancer patients [J]. Asia Pac J Clin Nutr, 2015, 24(4):591-597. http://cn.bing.com/academic/profile?id=13821a603608e6d0a14da1574704d730&encoded=0&v=paper_preview&mkt=zh-cn [5] Bouillanne O, Morineau G, Dupont C, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients[J]. Am J Clin Nutr, 2005, 82(4):777-783. doi: 10.1093/ajcn/82.4.777 [6] Cereda E, Klersy C, Pedrolli C, et al. The Geriatric Nutritional Risk Index predicts hospital length of stay and in-hospital weight loss in elderly patients[J]. Clin Nutr, 2015, 34(1):74-78. doi: 10.1016/j.clnu.2014.01.017 [7] Shoji F, Miura N, Matsubara T, et al. Prognostic significance of immune- nutritional parameters for surgically resected elderly lung cancer patients: a multicentre retrospective study[J]. Interact Cardiovasc Thorac Surg, 2018, 26(3):389-394. doi: 10.1093/icvts/ivx337 [8] Kushiyama S, Sakurai K, Kubo N, et al. The preoperative Geriatric Nutritional Risk Index predicts postoperative complications in elderly patients with gastric cancer undergoing gastrectomy[J]. In Vivo, 2018, 32(6):1667-1672. doi: 10.21873/invivo.11430 [9] Bo Y, Wang K, Liu Y, et al. The Geriatric Nutritional Risk Index predicts survival in elderly esophageal squamous cell carcinoma patients with radiotherapy[J]. PLoS One, 2016, 11(5):e155903. http://cn.bing.com/academic/profile?id=949aee0ab30f9372b385b58658037d6b&encoded=0&v=paper_preview&mkt=zh-cn [10] Wang J, Wu N, Zheng QF, et al. Evaluation of the 7th edition of the TNM classification in patients with resected esophageal squamous cell carcinoma[J]. World J Gastroenterol, 2014, 20(48):18397-18403. doi: 10.3748/wjg.v20.i48.18397 [11] Obesity: preventing and managing the global epidemic. Report of a WHO consultation[J]. World Health Organ Tech Rep Ser, 2000, 894:1- 253. http://d.old.wanfangdata.com.cn/OAPaper/oai_doaj-articles_ebbfb139ef0d06ef3ba146b5b2ecc278 [12] 乔乐乐, 王公平, 周博, 等.胃癌患者术前CRP/Alb比与淋巴结转移相关性的研究[J].中国肿瘤临床, 2017, 44(5):210-213. doi: 10.3969/j.issn.1000-8179.2017.05.246 [13] Zhang H, Shang X, Ren P, et al. The predictive value of a preoperative systemic immune-inflammation index and prognostic nutritional index in patients with esophageal squamous cell carcinoma[J]. J Cell Physiol, 2019, 234(2):1794-1802. doi: 10.1002/jcp.27052 [14] Gangadharan A, Choi SE, Hassan A, et al. Protein calorie malnutrition, nutritional intervention and personalized cancer care[J]. Oncotarget, 2017, 8(14):24009-24030. http://cn.bing.com/academic/profile?id=9c6fb84087d6dbcaf1aa86a2dd96fff6&encoded=0&v=paper_preview&mkt=zh-cn [15] Kawai H, Ota H. Low perioperative serum prealbumin predicts early recurrence after curative pulmonary resection for non- small- cell lung cancer[J]. World J Surg, 2012, 36(12):2853-2857. doi: 10.1007/s00268-012-1766-y [16] Anandavadivelan P, Lagergren P. Cachexia in patients with oesophageal cancer[J]. Nat Rev Clin Oncol, 2016, 13(3):185-198. doi: 10.1038/nrclinonc.2015.200 [17] Zhang H, Zhang B, Zhu K, et al. Preoperative albumin-to-globulin ratio predicts survival in patients with non-small-cell lung cancer after surgery[J]. J Cell Physiol, 2019, 234(3):2471-2479. doi: 10.1002/jcp.v234.3 [18] Chen Z, Shao Y, Wang K, et al. Prognostic role of pretreatment serum albumin in renal cell carcinoma: a systematic review and metaanalysis[J]. Onco Targets Ther, 2016, 9:6701-6710. doi: 10.2147/OTT [19] Zhang SS, Yang H, Luo KJ, et al. The impact of body mass index on complication and survival in resected oesophageal cancer: a clinical-based cohort and meta-analysis[J]. Br J Cancer, 2013, 109(11): 2894-2903. doi: 10.1038/bjc.2013.666 [20] 郭敏, 王翠, 张楠, 等.应用倾向值匹配法评价体质指数对食管鳞癌患者术后并发症及生存率的影响[J].中国肿瘤临床, 2018, 45(11): 589-594. doi: 10.3969/j.issn.1000-8179.2018.11.301 [21] Owczarek AJ, Choreza P, Arabzada H, et al. Kidney Function, Nutritional Status, and the Left Ventricle Dysfunction Are Associated with Serum Uric Acid Levels in Patients with Heart Failure with Reduced Ejection Fraction[J]. Ann Clin Lab Sci, 2018, 48(5):608-613. http://cn.bing.com/academic/profile?id=575ca88330bd82c8f978dc0d35a5b9d4&encoded=0&v=paper_preview&mkt=zh-cn [22] Shergill R, Syed W, Rizvi SA, et al. Nutritional support in chronic liver disease and cirrhotics[J]. World J Hepatol, 2018, 10 (10):685-694. doi: 10.4254/wjh.v10.i10.685 [23] Shoji F, Matsubara T, Kozuma Y, et al. Preoperative Geriatric Nutritional Risk Index: a predictive and prognostic factor in patients with pathological stage I non-small cell lung cancer[J]. Surg Oncol, 2017, 26(4):483-488. doi: 10.1016/j.suronc.2017.09.006 [24] Reynolds JV, Shou JA, Sigal R, et al. The influence of protein malnutrition on T cell, natural killer cell, and lymphokine-activated killer cell function, and on biological responsiveness to high-dose interleukin-2[J]. Cell Immunol, 1990, 128(2):569-577. doi: 10.1016/0008-8749(90)90049-W [25] Miyata H, Yano M, Yasuda T, et al. Randomized study of the clinical effects of omega-3 fatty acid-containing enteral nutrition support during neoadjuvant chemotherapy on chemotherapy-related toxicity in patients with esophageal cancer[J]. Nutrition, 2017, 33:204- 210. doi: 10.1016/j.nut.2016.07.004 -




 下载:
下载: