Prediction model for distant metastasis of breast cancer based on magnetic resonance imaging
-
摘要:
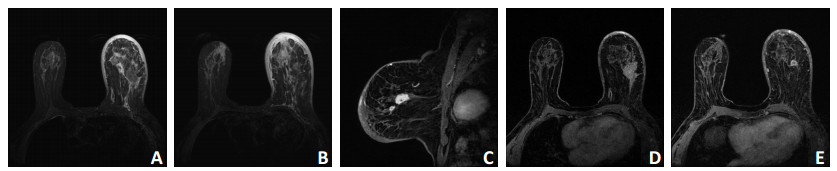
目的 建立基于平扫磁共振成像(magnetic resonance imaging,MRI)和动态对比增强(dynamic contrast enhanced,DCE)-MRI影像特征参数的乳腺癌远处转移预测模型。 方法 回顾性分析2011年1月至2016年12月3 032例于天津医科大学肿瘤医院行乳腺MRI检查并经病理证实为乳腺浸润性癌患者的临床资料,根据纳入标准筛选出转移组93例和非转移组186例。分析转移组远处转移部位与分子分型的关系,同时对两组MRI影像特征进行单因素分析及多因素Logistics回归分析,获得独立预测因子并建立预测模型。 结果 转移组中Luminal型、HER-2过表达型、三阴性乳腺癌最常见远处转移部位分别为骨、肝脏、肺脏。单因素分析结果显示,两组间的病变类型、是否多发、T1WI和T2WI信号均匀度及病灶最大径进行比较差异具有统计学意义(P < 0.05)。多因素Logistics回归分析结果显示,病变类型、是否多发、T2WI信号均匀度及病灶最大径为独立预测因子。根据独立预测因子建立的预测模型准确率、敏感度、特异度和受试者工作特征曲线(receiver operating characteristic,ROC)下面积(area under receiver operat? ing characteristic curve,AUC)分别为82.8%、85.7%、75.0%和0.801。 结论 基于MRI影像特征的模型对预测乳腺癌远处转移具有潜在价值。 Abstract:Objective To establish a prediction model for the distant metastasis of breast cancer based on qualitative magnetic resonance imaging (MRI) parameters. Methods A retrospective analysis of 3, 032 patients with breast MRI from January 2011 to December 2016 in Tianjin Medical University Cancer Institute and Hospital was conducted. After the confirmation of invasive breast cancer, the subjects were divided in 2 groups: metastasis and metastasis-free. A total of 93 patients were included in the metastasis group, and 186 patients without the presence of distant metastasis in the metastasis-free group. We analyzed the correlation between breast cancer molecular subtypes and distant metastasis in the metastasis group. Univariate and Logistic regression analyses of qualitative MRI features were performed for the groups. Subsequently, we used the results to establish prediction models. Results The results showed that hormone receptor-positive tumors (Luminal type) had a greater tendency to develop bone metastasis in the metastasis group. Triple-negative tumors showed a greater tendency to develop lung metastasis. Human epidermal growth factor receptor 2 gene overexpression cases were more likely to develop liver metastasis. The results of the univariate analysis showed that the type of lesion, multifocality or multicentricity of the cancer, T1-weighted signal uniformity, T2-weighted signal uniformity, and tumor size were statistically different between the groups (P < 0.05). The results of the logistic regression analysis showed that the type of lesion, multifocality or multicentricity of the cancer, T2-weighted signal uniformity, and tumor size were independent predictors of distant metastasis. Based on select independent predictors, we established a prediction model for the distant visceral metastasis of breast cancer. The accuracy, area under the curve, sensitivity, and specificity of the model were 82.8%, 0.801, 85.7%, and 75.0%, respectively. Conclusions The prediction model based on the clinical pathology and MRI features established in this study can predict the distant metastasis of breast cancer. -
Key words:
- breast cancer /
- neoplasm metastasis /
- magnetic resonance imaging (MRI) /
- prediction /
- molecular subtype
-
表 1 转移组和非转移组乳腺癌患者MRI表现特征比较

表 2 乳腺癌患者MRI表现特征Logistics多因素回归分析

-
[1] Huang Z, Sun B, Wu S, et al. A nomogram for predicting survival in patients with breast cancer brainmetastasis[J]. Oncol Lett, 2018, 15 (5):7090-7096. https://www.spandidos-publications.com/ol/15/5/7090 [2] 崔世恩, 储兵, 凌飞海.390例原发乳腺癌远处转移与分子分型关联性的10年回顾性分析[J].中国癌症杂志, 2015, 25(10):774-779. http://d.old.wanfangdata.com.cn/Periodical/zgazzz201510004 [3] 曹旭晨, 高宇.女性原发浸润性乳腺癌预后指数的研究[J].天津医科大学学报, 2005, 11(4):590-595. doi: 10.3969/j.issn.1006-8147.2005.04.027 [4] Li S, Zhao J, Zhu L, et al. Development and validation of a nomogram predicting the overall survival of stage Ⅳ breast cancer patients[J]. Cancer Med, 2017, 6(11):2586-2594. doi: 10.1002/cam4.2017.6.issue-11 [5] Song SE, Shin SU, Moon HG, et al. MR imaging features associated with distant metastasis- free survival of patients with invasive breast cancer: a case- control study[J]. Breast Cancer Res Treat, 2017, 162(3):559-569. doi: 10.1007/s10549-017-4143-6 [6] Kim S, Kim JY, Kim DH, et al. Analysis of phyllodes tumor recurrence according to the histologic grade[J]. Breast Cancer Res Treat, 2013, 141(3):353-363. doi: 10.1007/s10549-013-2684-x [7] Genre L, Roché H, Varela L, et al. External validation of a published nomogram for prediction of brain metastasis in patients with extracerebral metastatic breast cancer and risk regression analysis[J]. Eur J Cancer, 2017, 72:200-209. doi: 10.1016/j.ejca.2016.10.019 [8] Huang SY, Franc BL, Harnish RJ, et al. Exploration of PET and MRI radiomic features for decoding breast cancer phenotypes and prognosis[J]. NPJ Breast Cancer, 2018, 4(1):24. doi: 10.1038/s41523-018-0078-2 [9] 苗培田, 佟仲生, 郝春芳, 等.不同亚型转移性乳腺癌转移特点及预后分析[J].中国肿瘤临床, 2011, 38(4):228-231. http://www.cjco.cn/CN/abstract/abstract8588.shtml [10] Savci-Heijink CD, Halfwerk H, Hooijer GK, et al. Retrospective analysis of metastatic behaviour of breast cancer subtypes[J]. Breast Cancer Res Treat, 2015, 150(3):547-557. doi: 10.1007/s10549-015-3352-0 [11] 李芹, 牛庆亮, 杜汉旺, 等.肿块型与非肿块型乳腺癌ADC值、Ki67指数的对比分析[J].中国临床医学影像学杂志, 2018, 29(1):11-13. http://d.old.wanfangdata.com.cn/Periodical/zglcyxyxzz201801004 [12] Juan MW, Yu J, Peng GX, et al. Correlation between DCE- MRI radiomics features and Ki-67 expression in invasive breast cancer[J]. Oncol Lett, 2018, 16(4):5084-5090. http://cn.bing.com/academic/profile?id=237dfc82b4faa9765bee0fc6df7c879c&encoded=0&v=paper_preview&mkt=zh-cn [13] Ozal ST, Inci E, Gemici AA, et al. Can 3.0 Tesla diffusion tensor imaging parameters be prognostic indicators in breast cancer[J]? Clin Imaging, 2018, 51:240-247. doi: 10.1016/j.clinimag.2018.03.022 [14] Lynch SP, Lei X, Chavez-MacGregor M, et al. Multifocality and multicentricity in breast cancer and survival outcomes[J]. Ann Oncol, 2012, 23(12):3063-3069. doi: 10.1093/annonc/mds136 [15] Parikh J, Selmi M, Charles- Edwards G, et al. Changes in primary breast cancer heterogeneity may augment midtreatment MR imaging assessment of response to neoadjuvant chemotherapy[J]. Radiology, 2014, 272(1):100-112. doi: 10.1148/radiol.14130569 -




 下载:
下载: