-
摘要:
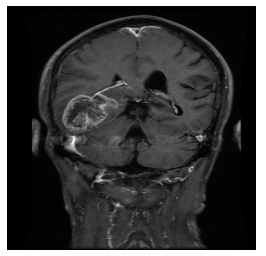
目的 探讨室管膜下区(subventricular zone, SVZ)受侵对脑胶质瘤预后的影响。 方法 回顾性分析江西省肿瘤医院2010年1月至2015年7月收治的175例经病理诊断为脑胶质瘤患者的临床资料, 其中WHOⅡ级59例, Ⅲ级59例, Ⅳ级57例; 根据术前MRI检查病灶与SVZ的位置关系, 分为SVZ受侵组(SVZ+)及SVZ未受侵组(SVZ-), 其中SVZ (+)组75例, SVZ (-)组100例, 比较两组的生存时间及复发模式。 结果 中位随访时间63个月; 5年总生存率(overall survival, OS)及无进展生存率(progression-free survival, PFS)分别为42.2%、37.5%;SVZ (+)组5年OS为20.9%, SVZ (-)组为57.1%(P< 0.001);而5年PFS分别为15.3%、44.1%(P< 0.001)。SVZ (+)组手术全切率更低(P< 0.001), 有更多大病灶(最大径≥ 5.0 cm)及Ⅳ级病例(P < 0.001, P=0.018)。全组共89例复发, SVZ (+)组总复发率为62.7%, SVZ (-)组为42.0%(P=0.007), 而远处复发率分别为21.3%、7.0%(P=0.004)。 结论 SVZ受侵是影响脑胶质瘤OS、PFS的不良预后因素, 且与低的全切率、大病灶及Ⅳ级病变呈正相关; SVZ受侵增加了总复发及远处复发概率。 Abstract:Objective To investigate the prognostic value of subventricular zone (SVZ) invasion in glioma patients. Methods The clinical data of 175 patients with glioma diagnosed based on pathology in Jiangxi Province Cancer hospital between January 2010 and July 2015 were analyzed retrospectively.There were 59 cases of World Health Organization (WHO) grade Ⅱ, 59 cases of WHO grade Ⅲ, and 57 cases of WHO grade Ⅳ at the first diagnosis.There were 75 cases of SVZ invasion (SVZ+) and 100 cases of SVZ non-invasion (SVZ-) according to preoperative magnetic resonance imaging.The survival outcomes of both cohorts were compared using the Logrank test.The correlation between the recurrence pattern and SVZ involvement was analyzed using Chi-square tests. Results The median follow-up time was 63 months.The 5-year overall survival (OS) and progression-free survival (PFS) rates were 42.2% and 37.5%, respectively.These were 20.9% and 15.3% in the SVZ+group, compared with 57.1% and 44.1% in the SVZ-group, respectively (P< 0.001 and P< 0.001, respectively).The SVZ+group had fewer cases of total resection, larger lesions (maximum diameter greater than 5.0 cm), and more cases of grade Ⅳ(P< 0.001, P< 0.001, and P=0.018, respectively).There were 89 cases of recurrence.The total recurrence rate was 62.7% in the SVZ+group, compared with 42.0% in the SVZ-group (P=0.007);the distant recurrence rates were 21.3% and 7.0%(P=0.004), respectively. Conclusions SVZ invasion is a poor prognostic factor for OS and PFS in gliomas, which is positively correlated with a low total resection rate, large lesions, and grade Ⅳ lesions, and increases the probability of total recurrence and distant recurrence. -
Key words:
- glioma /
- subventricular zone (SVZ) /
- prognosis
-
表 1 175例胶质瘤患者临床特征 n(%)

表 2 影响OS、PFS的单因素分析

表 3 影响OS、PFS的多因素分析

表 4 两组患者是否出现复发的比较 n(%)

表 5 两组患者复发部位的比较 n(%)

-
[1] 彭世义, 李艳萍, 陈志萍, 等.WHOⅡ级脑胶质瘤预后影响因素分析[J].中国肿瘤临床, 2018, 45(8):402-407. doi: 10.3969/j.issn.1000-8179.2018.08.374 [2] 吴帅, 李泽阳, 邱天明, 等.术中磁共振成像在脑胶质瘤中的应用[J].中华神经外科杂志, 2018, 34(4):333-337. doi: 10.3760/cma.j.issn.1001-2346.2018.04.003 [3] Altmann C, Keller S, Schmidt MHH. The role of SVZ stem cells in glioblastoma[J]. Cancers, 2019, 11(4):3390. [4] Androutsellis-Theotokis A, Leker RR, Soldner F, et al. Notch signalling regulates stem cell numbers in vitro and in vivo[J]. Nature, 2006, 442 (7104):823-826. doi: 10.1038/nature04940 [5] Groszer M. Negative regulation of neural stem/progenitor cell proliferation by the pten tumor suppressor gene in vivo[J]. Science, 2001, 294(5549):2186-2189. doi: 10.1126/science.1065518 [6] Wen B, Fu F, Hu L, et al. Subventricular zone predicts high velocity of tumor expansion and poor clinical outcome in patients with low grade astrocytoma[J]. Clin Neurol Neurosurg, 2018, 168(3):12-17. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=6d8d9a2c58da08a8eb98aedf16fa3234 [7] Mistry AM, Kelly PD, Gallant JN, et al. Comparative analysis of subventricular zone glioblastoma contact and ventricular entry during resection in predicting dissemination, hydrocephalus, and survival[J]. Neurosurgery, 2019, 6(3):144. [8] Chaichana KL, Mcgirt MJ, Frazier J, et al. Relationship of glioblastoma multiforme to the lateral ventricles predicts survival following tumor resection[J]. J Neurooncol, 2008, 89(2):219-224. doi: 10.1007/s11060-008-9609-2 [9] 国家卫生健康委员会医政医管局.脑胶质瘤诊疗规范(2018年版)[J].中华神经外科杂志, 2019, 35(3):217-239. doi: 10.3760/cma.j.issn.1001-2346.2019.03.001 [10] Chang EL, Avalos T, Chao C, et al. An evaluation of peritumoral edema in the clinical target volume delineation for radiotherapy of glioblastoma[J]. Int J Radiat Oncol Biol Phys, 2007, 68(1):144-150. doi: 10.1016/j.ijrobp.2006.12.009 [11] Wen PY, Macdonald DR, Reardon DA, et al. Updated response assessment criteria for high- grade gliomas: response assessment in neuro-oncology working group[J]. J Clin Oncol, 2010, 28(11):1963- 1972. doi: 10.1200/JCO.2009.26.3541 [12] Liu S, Wang Y, Fan X, et al. Anatomical involvement of the subventricularzone predicts poor survival outcome in low-grade astrocytomas[J]. PLoS One, 2016, 11(4):e0154539. doi: 10.1371/journal.pone.0154539 [13] Mistry AM, Dewan MC, White-Dzuro GA, et al. Decreased survival in glioblastomas is specific to contact with the ventricular-subventricular zone, not subgranular zone or corpus callosum[J]. J Neurooncol, 2017, 132(2):341-349. doi: 10.1007/s11060-017-2374-3 [14] Lim DA, Cha S, Mayo MC, et al. Relationship of glioblastoma multiforme to neural stem cell regions predicts invasive and multifocal tumor phenotype[J]. Neuro Oncol, 2007, 9(4):424-429. doi: 10.1215/15228517-2007-023 [15] Chen L, Chaichana KL, Kleinberg L, et al. Glioblastoma recurrence patterns near neural stem cell regions[J]. Radiother Oncol, 2015, 116 (2):294-300. doi: 10.1016/j.radonc.2015.07.032 [16] Ho J, Ondos J, Ning H, et al. Chemoirradiation for glioblastoma multiforme: the national cancer institute experience[J]. PLoS One, 2013, 8(8):e70745. doi: 10.1371/journal.pone.0070745 [17] Liang HK, Kuo SH, Wang CW, et al. Adverse prognosis and distinct progression patterns after concurrent chemoradiotherapy for glioblastoma with synchronous subventricular zone and corpus callosum invasion[J]. Radiother Oncol, 2016, 118(1):16-23. doi: 10.1016/j.radonc.2015.11.017 [18] Xingyi J, Guonan C, Xin Z, et al. AbCD133 modified αct1 loaded target magnetic mesoporous silica nano-drugcarriers can sensitizes glioma cancer stem cells to tmz and have therapeutic potential on tmz resistant glioblastoma[J]. J Biomed Nanotechnol, 2019, 15(7):1468-1481. doi: 10.1166/jbn.2019.2795 [19] Chen J, Li Y, Yu TS, et al. A restricted cell population propagates glioblastoma growth after chemotherapy[J]. Nature, 2012, 488(7412):522- 526. doi: 10.1038/nature11287 [20] Cuddapah VA, Robel S, Watkins S, et al. A neurocentric perspective on glioma invasion[J]. Nat Rev Neurosci, 2014, 15(7):455-465. doi: 10.1038/nrn3765 [21] Roelz R, Reinacher P, Jabbarli R, et al. Surgical ventricular entry is a key risk factor for leptomeningeal metastasis of high grade gliomas[J]. Sci Rep, 2015, 5:17758. doi: 10.1038/srep17758 [22] Adeberg S, Harrabi SB, Bougatf N, et al. Do increased doses to stem-cell niches during radiation therapy improve glioblastoma survival[J]? Stem Cells Int, 2016, 2016:8793462. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4939331/ [23] Kusumawidjaja G, Gan PZ, Ong WS, et al. Dose-escalated intensitymodulated radiotherapy and irradiation of subventricular zones in relation to tumor control outcomes of patients with glioblastoma multiforme[J]. Onco Targets Ther, 2016, 9:1115-1122. https://www.ncbi.nlm.nih.gov/pubmed/27042103 [24] Khalifa J, Tensaouti F, Lusque A, et al. Subventricular zones: new key targets for glioblastoma treatment[J]. Radiation Oncology, 2017, 12(1): 67. doi: 10.1186/s13014-017-0791-2 [25] Mathew BS, Kaliyath SB, Krishnan J, et al. Impact of subventricular zone irradiation on outcome of patients with glioblastoma[J]. J Can Res Ther 2018, 14:1202-1206. https://www.researchgate.net/publication/308769498_Impact_of_Subventricular_Zone_SVZ_Irradiation_on_Outcome_of_Patients_With_Glioblastoma_Multiforme [26] Muracciole X, El-Amine W, Tabouret E, et al. Negative survival impact of high radiation doses to neural stem cells niches in an idhwild-type glioblastoma population[J]. Front Oncol, 2018, 4(8):426. https://www.onacademic.com/detail/journal_1000040891500010_bdfd.html -




 下载:
下载: