Improved intercostal nerve block with ropivacaine in video-assisted thoracic surgery
-
摘要:
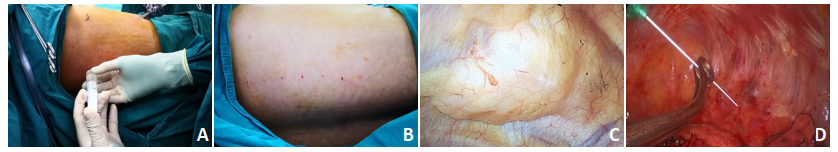
目的 比较胸腔镜手术后不同途径给予罗哌卡因肋间神经阻滞对患者术后镇痛效果。 方法 选取2018年8月至2018年11月天津医科大学肿瘤医院60例接受胸腔镜手术治疗的肺癌患者, 手术结束时使用0.25%罗哌卡因阻滞肋间神经, 采用改良式胸腔外经胸壁阻滞(试验组)和传统式胸腔内阻滞(对照组)。观察手术后12 h (T1)、24 h (T2)、48 h (T3)及72 h (T4)时两组患者静息时疼痛VAS评分及疼痛评分(Prince Henry Pain Scale, PHPS); 同时观察手术后追加吗啡剂量和相关不良反应事件。 结果 两组患者术后镇痛效果均较满意, 试验组术后T1~T4各时间点VAS和P-H疼痛评分均无显著性差异(P>0.05), 术后吗啡用量及带管时间两组无显著性差异(P>0.05), 试验组在穿刺后胸膜下血肿发生例数较少。 结论 胸腔镜下改良式罗哌卡因肋间神经阻滞与传统式胸腔内阻滞均能起到术后较好镇痛效果, 改良式肋间神经阻滞的方法具有操作简便, 并发症少的优点。 Abstract:Objective To compare two methods of injecting ropivacaine as an intercostal nerve blocker, and for postoperative pain control after video-assisted thoracic surgery (VATS) in lung cancer patients. Methods From August 2018 to November 2018, 60 patients who had undergone VATS with a diagnosis of lung cancer, were randomly assigned into two groups:control and test.After the surgery, the control group was injected with an intercostal nerve blocker (0.25% ropivacaine) via the inner thorax by the traditional method, and the test group was injected with ropivacaine via the outer thorax by an improved method.The pain scale was evaluated using the Visual Analogue Scale (VAS) and Prince Henry Pain Scale (PHPS) at 12 h (T1), 24 h (T2), 48 h (T3), and 72 h (T4) after the surgery.The dosage of administered morphine and the adverse effects of ropivacaine after surgery were also evaluated. Results Injecting ropivacaine to the intercostal nerve by means of both, outer and inner thoracic injection showed satisfied analgesia, as evaluated by VAS and PHPS scores, and there were no significant differences between the two methods at any time point of analysis (T1-T4, P>0.05).The dosage of administered morphine and the time with chest tube were similar (P>0.05) between the groups.However, there were a few cases of subpleural hemorrhage in the test group. Conclusions Intercostal nerve block with ropivacaine by means of both, outer and inner thoracic injection, showed satisfied analgesia, although, outer thoracic injection is more flexible with fewer complications. -
表 1 胸腔镜手术后患者疼痛情况VAS评估结果

表 2 胸腔镜手术后患者疼痛情况PHPS评估结果

表 3 胸腔镜手术后患者吗啡用量及术后带管时间的比较

-
[1] 中华医学会麻醉学分会.成人术后疼痛处理专家共识[J].临床麻醉学杂志, 2010, 26(3):190-196. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=lcmzxzz201003002 [2] Kwon S, Zhao L, Reddy R, et al. Evaluation of acute and chronic pain outcomes after robotic, video-assisted thoracoscopic surgery, or open anatomic pulmonary resection[J]. J Thorac Cardiovasc Surg, 2017, 154 (2):652-659. doi: 10.1016/j.jtcvs.2017.02.008 [3] 李跃, 宫立群, 徐锋, 等.罗哌卡因肋间神经阻滞对肺癌患者胸腔镜术后镇痛效果的影响[J].中国肿瘤临床2017, 44(12):605-607. doi: 10.3969/j.issn.1000-8179.2017.12.205 [4] Wang H, Li S, Liang N, et al. Postoperative pain experiences in Chinese adult patients after thoracotomy and video-assisted thoracic surgery [J]. J Clin Nurs, 2017, 26(17-18):2744-2754. doi: 10.1111/jocn.13789 [5] Shanthanna H, Aboutouk D, Poon E, et al. A retrospective study of open thoracotomies versus thoracoscopic surgeries for persistent postthoracotomy pain[J]. J Clin Anesth, 2016, (35):215-220. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=6cc5b3ceb3a177d3134b9c26fec2dbf5 [6] Yie J, Yang J, Wu C, et al. Patient-controlled analgesia (PCA) following video-assisted thoracoscopic lobectomy: comparison of epidural PCAand intravenous PCA[J]. Acta Anaesthesiol Taiwan, 2012, 50(3):92-95. doi: 10.1016/j.aat.2012.08.004 [7] Yoshioka M, Mori T, Kobayashi H, et al. The efficacy of epidural analgesia after video- assisted thoracoscopic surgery: a randomized control study[J]. Ann Thorac Cardiovasc Surg, 2006, 12(5):313-318. [8] Obuchi T, Yoshida Y, Moroga T, et al. Postoperative pain in thoracic surgery: re-evaluating the benefits of VATS when coupled with epidural analgesia[J]. J Thorac Dis, 2017, 9(11):4347-4352. doi: 10.21037/jtd.2017.09.133 [9] D'Andrilli A, Ibrahim M, Ciccone AM, et al. Intrapleural intercostal nerve block associated with mini-thoracotomy improves pain control after major lung resection[J]. Eur J Cardiothorac Surg, 2006, 29(5):790- 794. doi: 10.1016/j.ejcts.2006.01.002 [10] Ahmed Z, Samad K, Ullah H. Role of intercostal nerve block in reducing postoperative pain following video- assisted thoracoscopy: A randomized controlled trial[J]. Saudi J Anaesth, 2017, 11(1):54-57. doi: 10.4103/1658-354X.197342 [11] Gerner P. Postthoracotomy pain management problems[J]. Anesthesiol Clin, 2008, 26(2):355-367. doi: 10.1016/j.anclin.2008.01.007 [12] Piccioni F, Ragazzi R. Anesthesia and analgesia: how does the role of anesthetists changes in the ERAS program for VATS lobectomy[J]. J Vis Surg, 2018, 11: 4: 9. https://www.ncbi.nlm.nih.gov/pubmed/29445595 [13] Steinthorsdottir K, Wildgaard L, Hansen H, et al. Regional analgesia for video-assisted thoracic surgery: a systematic review[J]. Eur J Cardiothorac Surg, 2014, 45(6):959-66. doi: 10.1093/ejcts/ezt525 [14] Kim J, Kim T, Yang M, et al. Is intravenous patient controlled analgesia enough for pain control in patients who underwent thoracoscopy[J]? J Korean Med Sci, 2009, 24(5):930-935. doi: 10.3346/jkms.2009.24.5.930 [15] Chen L, Wu Y, Cai Y, et al. Comparison of programmed intermittent bolus infusion and continuous infusion for postoperative patientcontrolled analgesia with thoracic paravertebral block catheter: a randomized, double-blind, controlled trial[J]. Reg Anesth Pain Med, 2019, 44(2):240-245. doi: 10.1136/rapm-2018-000031 [16] Giang N, Van Nam N, Trung N, et al. Patient-controlled paravertebral analgesia for video-assisted thoracoscopic surgery lobectomy[J]. Local Reg Anesth, 2018, 22(11):115-121. [17] Fibla J, Molins L, Mier J, et al. The efficacy of paravertebral block using a catheter technique for postoperative analgesia in thoracoscopic surgery: a randomized trial[J]. Eur J Cardiothorac Surg, 2011, 40(4):907- 911. https://www.ncbi.nlm.nih.gov/pubmed/21316259 -




 下载:
下载: