-
摘要:
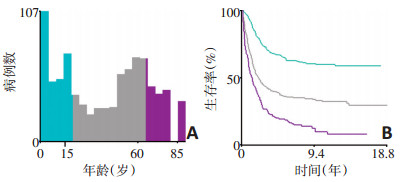
目的 构建列线图预测横纹肌肉瘤患者的1、3、5年生存率。 方法 从美国国立癌症研究所的监测、流行病学、结果数据库(SEER)数据库中收集1975年至2016年间诊断的横纹肌肉瘤患者,经筛选后最终获得861例符合条件的患者,采用单因素Kaplan-Meier法及多因素Cox模型分析确定横纹肌肉瘤患者独立的预后影响因素,然后将这些因素纳入并构建预测横纹肌肉瘤患者1、3、5年生存率的列线图。通过一致性指数(C-index)对所得列线图进行内部验证,检查其预测精度;同时,列线图预后模型的校正曲线一致性良好。 结果 年龄、病理类型、病理分级、总分期、手术、放疗及化疗均是横纹肌肉瘤患者的独立预后影响因素(P < 0.05),将这些因素纳入并成功构建了列线图。列线图的内部验证所得C指数为0.776。 结论 本次研究构建的横纹肌肉瘤患者生存风险的列线图具有良好的预测精度,有助于临床医师对横纹肌肉瘤患者预后作出较为准确的评估,也有利于对横纹肌肉瘤患者实施个体化诊疗。 Abstract:Objective To construct a nomogram for predicting the 1-year, 3-year, and 5-year survival of patients with rhabdomyosarcoma. Methods We retrieved data of patients diagnosed with rhabdomyosarcoma from The National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) database between 1975 and 2016. After screening, 861 eligible patients were selected. The univariate Kaplan-Meier method and multivariate Cox model were used to determine independent prognostic factors, which were then utilized to construct a nomogram to predict 1-year, 3-year, and 5-year survival of patients with rhabdomyosarcoma. The resulting nomogram was internally verified using the consistency index (C-index) to measure its predictive accuracy. Results Patient age, tumor histology, tumor grade, stage of the disease, surgery, radiotherapy, and chemotherapy were independent prognostic factors for patients with rhabdomyosarcoma (P < 0.05). Based on these factors, the nomogram was successfully constructed. The C-index value for internal validation of the nomogram was 0.776, and the calibration curves of the model were consistent. Conclusions The proposed nomogram is a reliable tool for accurate prognostic prediction in patients with rhabdomyosarcoma. It could be helpful for clinicians to individualize diagnosis, assess prognosis, and guide treatment plans for rhabdomyosarcoma patients. -
Key words:
- rhabdomyosarcoma /
- nomogram /
- prognosis /
- multivariate analysis
-
表 1 SEER数据库RMS患者总生存率的单因素及多因素分析

-
[1] Gatta G, Trama A, Capocaccia R, et al. Epidemiology of rare cancers and inequalities in oncologic outcomes[J]. Eur J Surg Oncol, 2019, 45(1):3-11. doi: 10.1016/j.ejso.2017.08.018 [2] Ognjanovic S, Linabery AM, Charbonneau B, et al. Trends in childhood rhabdomyosarcoma incidence and survival in the United States, 1975-2005[J]. Cancer, 2009, 115(18):4218-26. doi: 10.1002/cncr.24465 [3] Arndt CAS, Bisogno G, Koscielniak E. Fifty years of rhabdomyosarcoma studies on both sides of the pond and lessons learned[J]. Cancer Treat Rev, 2018, 68:94-101. doi: 10.1016/j.ctrv.2018.06.013 [4] PDQ Pediatric Treatment Editorial Board. Childhood Rhabdomyosarcoma Treatment (PDQ(R)):Health Professional Version[M]. US:National Cancer Institute, 2002. [5] Yang L, Yang J, Zhou X, et al. Development of a radiomics nomogram based on the 2D and 3D CT features to predict the survival of nonsmall cell lung cancer patients[J]. Eur Radiol, 2019, 29(5):2196-2206. doi: 10.1007/s00330-018-5770-y [6] Guo LW, Jiang LM, Gong Y, et al. Development and validation of nomograms for predicting overall and breast cancer-specific survival among patients with triple-negative breast cancer[J]. Cancer Manag Res, 2018, 10:5881-5894. doi: 10.2147/CMAR.S178859 [7] Wang C, Yang C, Wang W, et al. A Prognostic Nomogram for Cervical Cancer after Surgery from SEER Database[J]. J Cancer, 2018, 9(21):3923-3928. doi: 10.7150/jca.26220 [8] Bergamaschi L, Bertulli R, Casanova M, et al. Rhabdomyosarcoma in adults:analysis of treatment modalities in a prospective single-center series[J]. Med Oncol, 2019, 36(7):59. doi: 10.1007/s12032-019-1282-0 [9] Sun W, Chatterjee B, Shern JF, et al. Relationship of DNA methylation to mutational changes and transcriptional organization in fusionpositive and fusion-negative rhabdomyosarcoma[J]. Int J Cancer, 2019, 144(11):2707-2717. doi: 10.1002/ijc.32006 [10] Crist WM, Anderson JR, Meza JL, et al. Intergroup rhabdomyosarcoma study-Ⅳ:results for patients with nonmetastatic disease[J]. J Clin Oncol, 2001, 19(12):3091-3102. doi: 10.1200/JCO.2001.19.12.3091 [11] Raney RB, Anderson JR, Barr FG, et al. Rhabdomyosarcoma and undifferentiated sarcoma in the first two decades of life:a selective review of intergroup rhabdomyosarcoma study group experience and rationale for Intergroup Rhabdomyosarcoma Study V[J]. J Pediatr Hematol Oncol, 2001, 23(4):215-220. doi: 10.1097/00043426-200105000-00008 [12] Egas-Bejar D and Huh WW Rhabdomyosarcoma in adolescent and young adult patients:current perspectives[J]. Adolesc Health Med Ther, 2014, 5:115-125. http://cn.bing.com/academic/profile?id=2950727638113d3b6a655dc6086803d1&encoded=0&v=paper_preview&mkt=zh-cn [13] Crist WM, Garnsey L, Beltangady MS, et al. Prognosis in children with rhabdomyosarcoma:a report of the intergroup rhabdomyosarcoma studies Ⅰ and Ⅱ. Intergroup Rhabdomyosarcoma Committee[J]. J Clin Oncol, 1990, 8(3):443-452. doi: 10.1200/JCO.1990.8.3.443 [14] Cecchetto G, Carretto E, Bisogno G, et al. Complete second look operation and radiotherapy in locally advanced non-alveolar rhabdomyosarcoma in children:A report from the AIEOP soft tissue sarcoma committee[J]. Pediatr Blood Cancer, 2008, 51(5):593-597. doi: 10.1002/pbc.21702 [15] Eaton BR, McDonald MW, Kim S, et al. Radiation therapy target volume reduction in pediatric rhabdomyosarcoma:implications for patterns of disease recurrence and overall survival[J]. Cancer, 2013, 119(8):1578-1585. doi: 10.1002/cncr.27934 -




 下载:
下载: