Consensus on the clinical diagnosis, treatment, and prevention of chemotherapy-induced thrombocytopenia in China (2019 version)
-
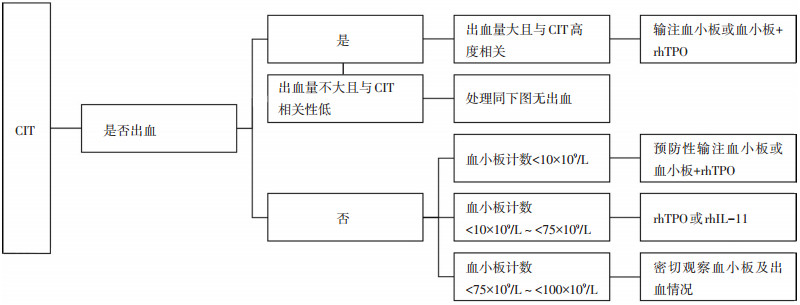
摘要: 肿瘤化疗相关性血小板减少症(chemotherapy-induced thrombocytopenia,CIT)为化疗常见的不良反应,发生率与肿瘤类型、治疗方案和化疗周期等有关。CIT可能导致化疗药物剂量降低或化疗时间延迟,甚至需要输注血小板,从而增加治疗费用、降低化疗效果和生存质量,影响预后。CIT的治疗主要包括输注血小板和给予促血小板生长因子。对高危患者进行一、二级预防有助于降低CIT的发生率和严重程度。基于近期文献及临床研究,中国抗癌协会肿瘤化疗专业委员会和肿瘤支持治疗专业委员会制订了《中国肿瘤化疗相关性血小板减少症专家诊疗共识(2019版)》,旨在为中国肿瘤学医师提供更合理的诊疗方案以帮助CIT患者改善肿瘤化疗所致血小板减少,提高患者生存质量。
-
关键词:
- 中国抗癌协会 /
- 专家共识 /
- 肿瘤化疗相关性血小板减少症 /
- 重组人白细胞介素11 /
- 重组人血小板生成素
Abstract: Chemotherapy-induced thrombocytopenia (CIT) is a common adverse reaction induced by chemotherapy, and its incidence is related to tumor type, therapeutic regimen, and duration of chemotherapy, etc. CIT may lead to dose reduction, delayed chemotherapy administration, and increased application of platelet transfusion, which increase the cost of treatment and reduces the efficacy of chemotherapy, resulting in a poor quality of life and prognosis. The main treatments of CIT include platelet transfusions and plateletstimulating factor injection. Primary and secondary preventions among high-risk patients may help reduce the incidence and severity of CIT. Based on a review of the literature and clinical trials, the expert committee of the China Anti-Cancer Association issued this consensus, aiming to support Chinese oncologists on the diagnosis and treatment of CIT in China. -
表 1 CIT分级标准

表 2 修订的WHO出血分级标准[15]

-
[1] 中国抗癌协会临床肿瘤学协作专业委员会.肿瘤化疗所致血小板减少症诊疗中国专家共识(2014版)[J].中华肿瘤杂志, 2014, 36(11):876-879. doi: 10.3760/cma.j.issn.0253-3766.2014.11.016 [2] Elting S, Rubenstein EB, Martin CG, et al. Incidence, cost, and outcomes of bleeding and chemotherapy dose modification among solid tumor patients with chemotherapy-induced thrombocytopenia[J]. J Clin Oncol, 2001, 19(4):1137-1146. doi: 10.1200/JCO.2001.19.4.1137 [3] Ten Berg MJ, van den Bemt PM, Shantakumar S, et al. Thrombocytopenia in adult cancer patients receiving cytotoxic chemotherapy:results from a retrospective hospital-based cohort study[J]. Drug safety, 2011, 34(12):1151-1160. doi: 10.2165/11594310-000000000-00000 [4] Castaman G, Pieri L. Management of thrombocytopenia in cancer[J]. Throm Res, 2018, 164(Suppl 1):S89-S93. http://d.old.wanfangdata.com.cn/Periodical/zhzl201809014 [5] Weycker D, Hatfield M, Grossman A, et al. Risk and consequences of chemotherapy-induced thrombocytopenia in US clinical practice[J]. BMC cancer, 2019, 19(1):151. doi: 10.1186/s12885-019-5354-5 [6] Machlus KR, Thon JN, Italiano JE, et al. Interpreting the developmental dance of the megakaryocyte:a review of the cellular and molecular processes mediating platelet formation[J]. Br J Haematol, 2014, 165(2):227-236. doi: 10.1111/bjh.12758 [7] Beg MS, Komrokji RS, Ahmed K, et al. Oxaliplatin-induced immune mediated thrombocytopenia[J]. Cancer Chemother Pharmacol, 2008, 62(5):925-927. doi: 10.1007/s00280-007-0675-5 [8] Zorzi D, Laurent A, Pawlik TM, et al. Chemotherapy-associated hepatotoxicity and surgery for colorectal liver metastases[J]. Br J Surg, 2007, 94(3):274-286. doi: 10.1002/bjs.5719 [9] Wu Y, Aravind S, Ranganathan G, et al. Anemia and thrombocytopenia in patients undergoing chemotherapy for solid tumors:a descriptive study of a large outpatient oncology practice database, 2000-2007[J]. Clin Ther, 2009, 3(1 Pt 2):2416-2432. [10] Hassan BA, Yusoff ZB, Hassali MA, et al. Treatment patterns and outcomes in management of solid cancer patients suffering from thrombocytopenia in Penang hospital[J]. Asian Pacific J Cancer Prev, 2011, 12(11):2841-2845. [11] Hitron A, Steinke D, Sutphin S, et al. Incidence and risk factors of clinically significant chemotherapy-induced thrombocytopenia in patients with solid tumors[J]. J Oncol Pharm Pract, 2011, 17(4):312-319. doi: 10.1177/1078155210380293 [12] 中国临床肿瘤学会肿瘤化疗所致血小板减少症共识专家委员会.肿瘤化疗所致血小板减少症诊疗中国专家共识(2018版)[J].中华肿瘤杂志, 2018, 40(9):714-720. doi: 10.3760/cma.j.issn.0253-3766.2018.09.014 [13] CTCAE v5.0, Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. 2017: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. [14] Kaushansky K. The thrombocytopenia of cancer. Prospects for effective cytokine therapy[J]. Hematol Oncol Clin North Am, 1996, 10(2):431-455. doi: 10.1016/S0889-8588(05)70346-4 [15] Stanworth SJ, Estcourt LJ, Powter G, et al. A no-prophylaxis platelet transfusion strategy for hematologic cancers[J]. New Engl J Med, 2013, (368):1771-1780. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=ddf0ae47d3a36397d61c6f06c29839dc [16] Schiffer CA, Bohlke K, Delaney M, et al. Platelet transfusion for patients with cancer:American society of clinical oncology clinical practice guideline update[J]. J Clin Oncol, 2018, 36(3):283-299. doi: 10.1200/JCO.2017.76.1734 [17] 白春梅, 徐光勋, 赵永强, 等.重组人血小板生成素治疗实体肿瘤患者化疗后血小板减少的多中心临床试验[J].中国医学科学院学报, 2004, 26(4):437-441. doi: 10.3321/j.issn:1000-503X.2004.04.020 [18] Vadhan-Raj S, Murray LJ, Bueso-Ramos C, et al. Stimulation of megakaryocyte and platelet production by a single dose of recombinant human thrombopoietin in patients with cancer[J]. Ann Intern Med, 1997, 126(9):673-681. doi: 10.7326/0003-4819-126-9-199705010-00001 [19] 赵永强, 姜杰玲, 焦力, 等.重组人血小板生成素临床耐受性试验[J].中华医学杂志, 2001, 81(24):1508-1511. doi: 10.3760/j:issn:0376-2491.2001.24.012 [20] 华宝来, 赵永强, 朱铁楠, 等.血小板减少患者皮下注射重组人血小板生成素后抗体生成的动态监测[J].血栓与止血, 2005, 11(2):59-61. doi: 10.3969/j.issn.1009-6213.2005.02.004 [21] 储大同, 徐兵河, 宋三泰, 等.重组人白细胞介素11(迈格尔)对化疗引起骨髓抑制肿瘤病人的促血小板生成作用[J].中国实验血液学杂志, 2001, 9(4):314-317. doi: 10.3969/j.issn.1009-2137.2001.04.007 [22] 方静, 张荣艳, 肖承京.白细胞介素-11的细胞生物学作用及防治疾病的研究进展[J].实用临床医学, 2005, 6(8):150-152. doi: 10.3969/j.issn.1009-8194.2005.08.089 [23] Liu XG, Bai XC, Chen FP, et al. Chinese guidelines for treatment of adult primary immune thrombocytopenia[J]. Int J Hematol, 2018, 107(6):615-623. doi: 10.1007/s12185-018-2445-z [24] 陈博, 李涛, 张军, 等.重组人血小板生成素治疗同步放化疗实体瘤患者血小板减少的临床疗效观察[J].癌症进展, 2012, 2012(10):2. http://d.old.wanfangdata.com.cn/Periodical/azjz201202003 [25] 尹预真, 叶丽霖, 杨静, 等.重组人血小板生成素联合重组人白介素-11治疗恶性肿瘤放化疗后血小板下降的临床效果[J].武汉大学学报(医学版), 2014, 35(6):967-968. http://d.old.wanfangdata.com.cn/Periodical/hubeiykdxxb201406038 [26] 万里新, 单丽红, 王旸, 等.重组人白介素-11治疗恶性肿瘤放化疗后血小板减少28例[J].郑州大学学报(医学版), 2007, 42(5):966-967. doi: 10.3969/j.issn.1671-6825.2007.05.058 [27] 任天舒, 张岩, 曲佳鑫, 等.重组人血小板生成素与重组人白细胞介素11治疗血小板减少症疗效与安全性的Meta分析[J].药物流行病学杂志, 2016, 25(1):6-10. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=ywlxbxzz201601003 [28] Emmons RV, Reid DM, Cohen RL, et al. Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction[J]. Blood, 1996, 87(10):4068-4071. doi: 10.1182/blood.V87.10.4068.bloodjournal87104068 [29] Wang Z, Fang X, Huang H, et al. Recombinant human thrombopoietin (rh-TPO) for the prevention of severe thrombocytopenia induced by high-dose cytarabine:a prospective, randomized, selfcontrolled study[J]. Leuk Lymph, 2018, 59(12):2821-2828. doi: 10.1080/10428194.2018.1459605 [30] Vadhan-Raj S, Patel S, Bueso-Ramos C, et al. Importance of predosing of recombinant human thrombopoietin to reduce chemotherapy-induced early thrombocytopenia[J]. J Clin Oncol, 2003, 21(16):3158-3167. doi: 10.1200-JCO.2003.08.003/ [31] Vadhan-Raj S, Verschraegen CF, Bueso-Ramos C, et al. Recombinant human thrombopoietin attenuates carboplatin-induced severe thrombocytopenia and the need for platelet transfusions in patients with gynecologic cancer[J]. Ann Intern Med, 2000, 132(5):364-368. http://cn.bing.com/academic/profile?id=506b59bacffcfcf43331475e0c1554f2&encoded=0&v=paper_preview&mkt=zh-cn [32] 徐云华, 成柏君, 陆舜.短程间歇预防性给予重组人血小板生成素治疗肺癌化疗诱导的严重血小板减少的疗效[J].中华肿瘤杂志, 2011, 33(5):395-399. doi: 10.3760/cma.j.issn.0253-3766.2011.05.021 [33] 刘自建, 骆泉湘, 刘芝兰.重组人白细胞介素-11治疗实体瘤化疗所致血小板减少的疗效观察[J].中国肿瘤临床与康复, 2018, 25(04):439-442. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgzllcykf201804016 [34] Ellis M, Zwaan F, Hedstrom U, et al. Recombinant human interleukin 11 and bacterial infection in patients with[correction of] haematological malignant disease undergoing chemotherapy:a double-blind placebo-controlled randomised trial[J]. Lancet, 2003, 361(9354):275-280. doi: 10.1016/S0140-6736(03)12322-7 [35] Wang KF, Pan HM, Lou HZ, et al. Interleukin-11-induced capillary leak syndrome in primary hepatic carcinoma patients with thrombocytopenia[J]. BMC Cancer, 2011, (11):204. http://d.old.wanfangdata.com.cn/OAPaper/oai_doaj-articles_4b553d3502df468eb34d1487c25d63e2 [36] 胡南华.重组人白细胞介素11诱发急性心力衰竭[J].临床合理用药杂志, 2013, 6(05):138-139. doi: 10.3969/j.issn.1674-3296.2013.05.126 [37] Wu Q, Ren J, Wu X, et al. Recombinant human thrombopoietin improves platelet counts and reduces platelet transfusion possibility among patients with severe sepsis and thrombocytopenia:a prospective study[J]. J Crit Care, 2014, 29(3):362-366. doi: 10.1016/j.jcrc.2013.11.023 [38] 侯明, 李曼, 靳征.重组人血小板生成素注射液上市后不良反应监测研究[J].中国新药与临床杂志, 2015, 34(08):642-646. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zgxyylczz201508018 -




 下载:
下载: