Growth pattern, tumor budding and CD8+T lymphocyte infiltration in colorectal adenocarcinoma invasive margins: association with clinicopathological features
-
摘要:
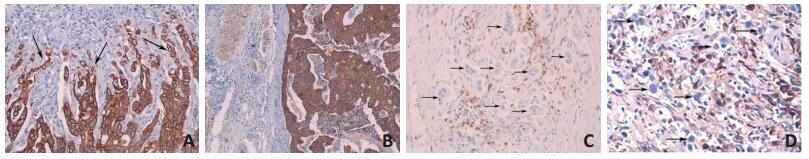
目的 观察结直肠腺癌侵袭性前缘的生长方式,计数肿瘤细胞巢出芽的数量和CD8+T淋巴细胞浸润的数量,探讨以上参数与相关临床病理学特征的关系。 方法 收集2008年1月至2019年12月在河西学院附属张掖人民医院院行手术切除的126例原发性结直肠腺癌患者的石蜡包埋样本,运用免疫组织化学方法对126例病理切片进行染色,广谱CK用于标记肿瘤细胞巢出芽,CD8标记T淋巴细胞进行评估。 结果 结直肠腺癌侵袭性前缘的浸润性生长方式,高级别肿瘤细胞巢出芽与肿瘤大小病理分期(pT)(P=0.029,P < 0.001),淋巴结转移病理分期(pN)(P < 0.001,P=0.023)及脉管浸润相关(P < 0.001,P < 0.001);高级别肿瘤细胞巢出芽与肿瘤组织学低分化程度相关(P < 0.001);高级别CD8+T淋巴细胞浸润可能与阻碍肿瘤细胞淋巴结转移相关(P=0.050)。 结论 结直肠腺癌侵袭性前缘的浸润性生长方式,高级别肿瘤细胞巢出芽与患者预后相关,两种组织学形态特征易于观察,可重复性好,借助于广谱CK免疫组织化学染色,可作为判断患者预后的指征。 Abstract:Objective The aim of this study was to explore the correlation between the clinicopathological characteristics of colorectal adenocarcinoma and the growth pattern, tumor budding, and CD8+T lymphocyte infiltration in anterior invasive margins, and to assess their value as prognostic indicators. Methods Paraffin embedded samples were collected from 126 patients with primary colorectal adenocarcinoma who underwent surgical resection in Zhangye People's Hospital Affiliated to Hexi College from January 2008 to December 2019. A total of 126 pathological sections were stained by immunohistochemistry. Anti-cytokeratin antibodies were used to mark tumor cell budding and anti-CD8 antibody markers T lymphocytes were evaluated. Results In colorectal adenocarcinoma, infiltrative growth patterns and highgrade tumor budding in invasive margins were significantly associated with pathological stage of tumor size (pT) (P=0.029 and P < 0.001, respectively), pathological stage of lymph node metastasis (pN) (P < 0.001 and P=0.023, respectively) and vessel infiltration (P < 0.001 and P < 0.001, respectively). Furthermore, high-grade CD8+T lymphocyte infiltration was associated with the absence of lymph node metastases (P=0.050). Conclusion Infiltrative growth patterns and high-grade tumor budding in colorectal adenocarcinoma invasive margins were correlated with patient prognosis. Importantly, these two features are easily detectable (with the help of pan-cytokeratin immunohistochemistry staining), in a reproducible manner. Therefore, we propose that they could be used as prognostic indicators in colorectal adenocarcinoma patients. -
Key words:
- colorectal adenocarcinoma /
- infiltrative growth /
- tumor budding /
- CD8+T lymphocytes
-
表 1 患者的临床病理学特征

表 2 肿瘤组织前缘肿瘤细胞巢出芽数和CD8+T细胞数及前缘生长方式与临床病理学特征的关系

-
[1] Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide:sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer, 2015, 136(5):359-386. http://cn.bing.com/academic/profile?id=92998753a0e7f31e127db34e72d37cd5&encoded=0&v=paper_preview&mkt=zh-cn [2] Amin M, Edge S, Greene F, et al. AJCC cancer staging manual. 8th ed[M]. New York, NY:Springer, 2017:251-265. https://www.springer.com/gp/book/9783319406176 [3] Jass JR, Ajioka Y, Allen JP, et al. Assessment of invasive growth pattern and lymphocytic infiltration in colorectal cancer[J]. Histopathology, 1996, 28(6):543-548. doi: 10.1046-j.1365-2559.1996.d01-467.x/ [4] Cho SJ, Kakar S. Tumor budding in colorectal carcinoma:translating a morphologic score into clinically meaningful results[J]. Arch Pathol Lab Med, 2018, 142(8):952-957. http://cn.bing.com/academic/profile?id=5058a7c3051c7a7241f67e1a2cffbff9&encoded=0&v=paper_preview&mkt=zh-cn [5] Berg KB, Schaeffer DF. Tumor budding as a standardized parameter in gastrointestinal carcinomas:more than just the colon[J]. Mod Pathol, 2018, 31(6):862-872. http://cn.bing.com/academic/profile?id=4882b73b3b6e3e3e475a2ddef303285b&encoded=0&v=paper_preview&mkt=zh-cn [6] Karamitopoulou E, Zlobec I, Kolzer V, et al. Proposal for a 10-highpower-fields scoring method for the assessment of tumor budding in colorectal cancer[J]. Modern Pathology, 2013, 26(2):295-301. https://www.nature.com/articles/modpathol2012155 [7] Lugli A, Karamitopoulou E, Panayiotides I, et al. CD8+ lymphocytes/tumour-budding index:an independent prognostic factor representing a 'pro-/anti-tumour' approach to tumour host interaction in colorectal cancer[J]. Br J Cancer, 2009, 101(8):1382-1392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2768462/ [8] Kim BH, Kim JM, Kang GH, et al. Standardized pathology report for colorectal cancer, 2nd edition[M]. J Pathol Transl Med, 2020, 54:1-19. [9] Zlobec I, Baker K, Minoo P, et al. Tumor border configuration added to TNM staging better stratifies stage Ⅱ colorectal cancer patients into prognostic subgroups[J]. Cancer, 2009, 115(17):4021-4029. https://pubmed.ncbi.nlm.nih.gov/19517467/ [10] Lugli A, Kirsch R, Ajioka Y, et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016[J]. Mod Pathol, 2017, 30(9):1299-1311. http://cn.bing.com/academic/profile?id=0f9f9575cb6f1b0f2296668931448131&encoded=0&v=paper_preview&mkt=zh-cn [11] Choi HJ, Park KJ, Shin JS, et al. Tumor budding as a prognostic marker in stage-III rectal carcinoma[J]. Int J Colorectal Dis, 2007, 22(8):863-868. http://cn.bing.com/academic/profile?id=b00a201381b5352e37cd8006c5f58a53&encoded=0&v=paper_preview&mkt=zh-cn [12] Deb B, Jacob SE. Predictive power of tumour budding for lymph node metastasis in colorectal carcinomas:A retrospective study[J]. Indian J Med Res, 2019, 150(6):635-639. http://cn.bing.com/academic/profile?id=f8ca04ac760344c377a2b8cc245ca96f&encoded=0&v=paper_preview&mkt=zh-cn [13] Dawson H, Blank A, Zlobec I, et al. Potential clinical scenarios of tumour budding in colorectal cancer[J]. Acta Gastroenterol Belg, 2019, 82(4):515-518. http://cn.bing.com/academic/profile?id=8e4bae68e316eb3ce65a40ad8dc323ab&encoded=0&v=paper_preview&mkt=zh-cn [14] Pages F, Berger A, Camus M, et al. Effector memory T cells, early metastasis, and survival in colorectal cancer[J]. N Engl J Med, 2005, 353(25):2654-2666. doi: 10.1056-NEJMoa051424/ [15] Mittal D, Lepletier A, Madore J, et al. CD96 Is an immune checkpoint that regulates CD8+T-cell antitumor function[J]. Cancer Immunol Res, 2019, 7(4):559-571. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=ce2af30dff88e0ff93a4088f93971ba0 [16] Zabijak L, Attencourt C, Guignant C, et al. Increased tumor infiltration by mucosal-associated invariant T cells correlates with poor survival in colorectal cancer patients[J]. Cancer Immunol Immunother, 2015, 64(12):1601-1608. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=46c4cf6f325963756cfb62e576905912 [17] Ogino S, Giannakis M. Immunoscore for (colorectal) cancer precision medicine[J]. Lancet, 2018, 391(10135):2084-2086. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=9f91488e3b6bcd49f759b3706d41473c -




 下载:
下载: