Comparative study of laparoscopic radical right hemicolectomy via the head-tail and medial approaches
-
摘要:
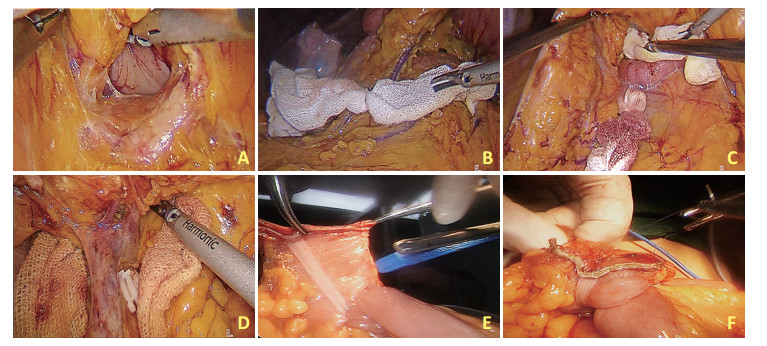
目的 探讨头尾联合入路和内侧入路在腹腔镜根治性右半结肠切除术的临床近期疗效及并发症。 方法 回顾性分析2015年1月至2019年12月期间由徐州医科大学附属医院收治的91例腹腔镜根治性右半结肠切除术患者的临床资料,分为50例接受头尾联合入路组和41例接受内侧入路组。针对两组入路手术时间、术中出血量、Henle干及其属支损伤率、因Henle干及其属支损伤致中转开腹率、淋巴结清扫数量、阳性淋巴结数量、术后肠功能恢复时间、腹腔引流管拔除时间、术后住院时间及术后并发症等临床指标评价并分析头尾联合入路的潜在优势。 结果 头尾联合入路组在手术时间上显著短于内侧入路组[180(150~188)min vs.210(180~255)min,P < 0.05]、术中出血量显著少于内侧入路组[50(50~50)mL vs.100(50~100)mL,P < 0.05]、Henle干及其属支损伤率显著低于内侧入路组[0例vs.6例,P < 0.05]。两组因Henle干及其属支损伤致中转开腹率、淋巴结清扫数量、阳性淋巴结数量、术后肠功能恢复时间、腹腔引流管拔除时间、术后住院时间及术后淋巴漏等并发症发生情况差异均无统计学意义(均P>0.05)。 结论 腹腔镜头尾联合入路能显著减少术中出血量、缩短手术时间、降低Henle干属支血管损伤率,有较高的手术安全性,值得临床进一步推广应用。 Abstract:Objective To investigate the short-term clinical efficacy and complications of laparoscopic radical right hemicolectomy via the head-tail and medial approaches. Methods Clinical data of 91 patients admitted for laparoscopic radical right hemicolectomy at Affiliated Hospital of Xuzhou Medical University between January 2015 and December 2019 were retrospectively analyzed. Of those patients, 50 and 41 patients underwent laparoscopic radical right hemicolectomy via the head-tail and medial approaches, respectively. According to the clinical indicators such as operation time, amount of intraoperative blood loss, rate of injury of Henle trunk and its branches (an indicator of conversion to laparotomy), number of lymph nodes dissected, number of positive lymph nodes, postoperative intestinal function recovery time, postoperative abdominal drainage tube removal time, postoperative hospitalization time, and postoperative complications, the potential advantages of laparoscopic radical right hemicolectomy via the head-tail approach were evaluated and analyzed. Results The operation time was significantly shorter[180 (150-188) min vs. 210 (180-255) min, P < 0.05], amount of intraoperative blood loss was significantly smaller[50 (50-50) mL vs. 100 (50-100) mL], P < 0.05), and rates of injury of Henle trunk and its branches (0 case vs. 6 cases, P < 0.05) were significantly lower in the head-tail approach group than in the medial approach group. We found no statistically significant differences between the two groups with the conversion rate to laparotomy due to injuries of Henle trunk and its branches, number of lymph nodes dissected, number of positive lymph nodes, postoperative intestinal function recovery time, postoperative abdominal drainage tube removal time, postoperative hospitalization time, postoperative lymph leakage, and other complications (P>0.05). Conclusions Compared with the commonly used medial approach in clinical practice, laparoscopic radical right hemicolectomy via the head-tail approach showed obvious improvement with respect to operative time, amount of intraoperative blood loss, and the injury rate of Henle trunk and its branches. Thus, the head-tail approach had higher operative safety and is thus worthy of further clinical application. -
Key words:
- combined head-tail approach /
- medial approach /
- laparoscope /
- right colon cancer /
- radical resection
-
表 1 两组患者基本资料比较

表 2 两组患者肿瘤相关资料比较
例 
表 3 两组患者术中观察指标比较

表 4 两组患者术后观察指标比较

-
[1] Wells KO. Minimally invasive colon cancer surgery[J]. Surg Oncol Clin N Am, 2019, 28(2):285-296. doi: 10.1016/j.soc.2018.11.004 [2] Hu W, Yang Y, Li X, et al. Multiomics approach reveals distinct differences in left and right-sided colon cancer[J]. Mol Cancer Res:MCR, 2018, 16(3):476-485. doi: 10.1158/1541-7786.MCR-17-0483 [3] Geiger TM. Colorectal cancer screening and diagnosis:a patientcentered approach to understanding avoidance[J]. Dis Colon Rectum, 2018, 61(4):417-418. doi: 10.1097/DCR.0000000000000968 [4] Alsabilah JF, Razvi SA, Albandar MH. Intraoperative archive of right colonic vascular variability aids central vascular ligation and redefines gastrocolic trunk of henle variants[J]. Dis Colon Rectum, 2017, 60(1):22-29. doi: 10.1097/DCR.0000000000000720 [5] Chaouch MA, Dougaz MW, Bouasker I, et al. Laparoscopic versus open complete mesocolon excision in right colon cancer:a systematic review and meta-analysis[J]. World J Surg, 2019, 43(12):3179-3190. doi: 10.1007/s00268-019-05134-4 [6] Heald RJ, Husband EM. The mesorectum in rectal cancer surgery——the clue to pelvic recurrence[J]? Br J Surg, 1982, 69(10):613-616. doi: 10.1002/bjs.1800691019 [7] Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer:complete mesocolic excision and central ligation——technical notes and outcome[J]. Colorectal Dis, 2009, 11(4):354-364. doi: 10.1111/j.1463-1318.2008.01735.x [8] Takahashi H, Takemasa I, Haraguchi N, et al. The single-center experience with the standardization of single-site laparoscopic colectomy for right-sided colon cancerJ[]. Surg Today, 2017, 47(8):966-972. doi: 10.1007/s00595-016-1457-7 [9] 揭志刚.腹腔镜右半结肠癌CME切除术的意义及利弊分析[J].中华普外科手术学杂志(电子版), 2018, 12(3):194-197. doi: 10.3877/cma.j.issn.1674-3946.2018.03.004. [10] Peltrini R, Luglio G, Pagano G, et al. Gastrocolic trunk of Henle and its variants:review of the literature and clinical relevance in colectomy for right-sided colon cancer[J]. Surg Radiol Anat, 2019, 41(8):879-887. doi: 10.1007/s00276-019-02253-4 [11] Osawa T, Komatsu S, Ishiguro S. Anatomy of the right colic vein and pancreaticoduodenal branches:a surgical landmark for laparoscopic complete mesocolic excision of the right colon[J]. Surg Radiol Anat, 2018, 40(4):423-429. doi: 10.1007/s00276-018-1994-4 [12] Bates DDB, Paroder V, Lall C, et al. Complete mesocolic excision and central vascular ligation for right colon cancer:an introduction for abdominal radiologists[J]. Abdom Radiol (NY), 2019, 44(11):3518-3526. doi: 10.1007/s00261-019-02037-9 [13] Xie D, Yu C, Gao C, et al. An optimal approach for laparoscopic d3 lymphadenectomy plus complete mesocolic excision (D3+CME) for right-sided colon cancer[J]. Ann Surg Oncol, 2017, 24(5):1312-1313. doi: 10.1245/s10434-016-5722-1 [14] Alsabilah J, Kim WR. Vascular structures of the right colon:incidence and variations with their clinical implications[J]. Scand J Surg, 2017, 106(2):107-115. doi: 10.1177/1457496916650999 [15] 郑民华, 马君俊.腹腔镜右半结肠癌根治术的难点与争议[J].中华普外科手术学杂志(电子版), 2018, 12(3):181-184. doi: 10.3877/cma.j.issn.1674-3946.2018.03.001. [16] 江晓锋, 朱冬云, 孔德灿, 等.应用门静脉增强CT静脉成像观察胃结肠静脉干及相关血管解剖变异的研究[J].中华胃肠外科杂志, 2019, 22(10):990-996. doi: 10.3760/cma.j.issn.1671-0274.2019.10.016 [17] Freund MR, Goldin I. Superior mesenteric vein injury during oncologic right colectomy:current vascular repair modalities[J]. Vasc Endovascular Surg, 2018, 52(1):11-15. doi: 10.1177/1538574417739749 [18] Stefura T, Kacprzyk A, Droś J, et al. The venous trunk of henle (gastrocolic trunk):A systematic review and meta-analysis of its prevalence, dimensions, and tributary variations[J]. Clin Anat, 2018, 31(8):1109-1121. doi: 10.1002/ca.23228 [19] 汤思哲, 王仆, 田斐, 等.伴血管变异的腹腔镜右半结肠癌根治术个体化手术入路的多学科临床探讨[J].中国肿瘤临床, 2019, 46(8):412-415. doi: 10.3969/j.issn.1000-8179.2019.08.154 -




 下载:
下载: