Consensus on the perioperative pain management of cancer patients in China (2020 edition)
-
摘要: 肿瘤切除术是绝大多数早中期实体肿瘤治疗的基础,肿瘤切除术后常伴随持续的疼痛。手术创伤和疼痛可引起炎症、下丘脑-垂体轴激活和交感系统过度反应发生。这些因素会影响肿瘤患者的免疫能力,导致免疫抑制。围术期有效的疼痛管理可以优化肿瘤患者的免疫功能,对肿瘤患者术后康复也具有重要意义。因此,中国抗癌协会肿瘤麻醉与镇痛专业委员会组织专家制定我国肿瘤患者围术期疼痛管理的专家共识,目的是为肿瘤患者术后急性疼痛管理提供基于证据的临床建议。本共识为学术性建议,仅限于指导肿瘤患者术后急性疼痛管理,不适用慢性疼痛或肿瘤导致的癌性疼痛。Abstract: Surgical tumor excision is a cornerstone of primary cancer treatment, and persistent postoperative pain is common after most surgical procedures. Surgical trauma and pain can cause inflammation, hypothalamic-pituitary axis activation, and sympathetic system over-reactivity. These factors, acting either separately or in combination, affect anti-tumor immunity and promote postoperative immunosuppression. Effective management of perioperative pain may help to modulate the unwanted consequences of the stress response on the immune system and improve outcomes. Based on the recent literature and clinical studies, experts from The Society of Oncological Anesthesia and Analgesia, Chinese Anti-Cancer Association have developed this consensus on the perioperative pain management of cancer patients in China (2020 edition). This consensus aims to provide evidence-based clinical recommendations for the acute pain management of cancer patients postoperatively. It does not apply to chronic pain or pain caused by cancer.
-
Key words:
- expert consensus /
- perioperative pain management /
- antitumor immunity /
- analgesic
-
表 1 疼痛评估方法

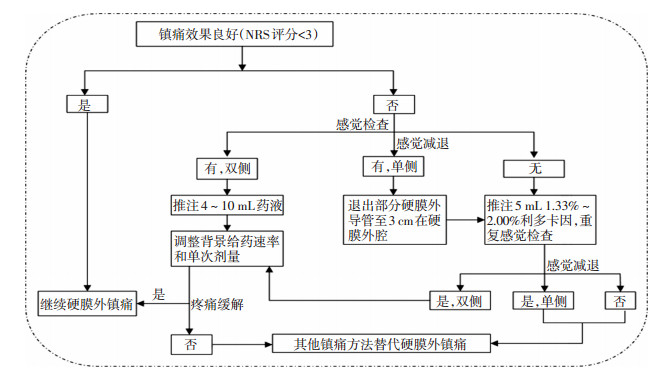
表 2 硬膜外镇痛药物和输注浓度

-
[1] Wu CL, Raja SN. Treatment of acute postoperative pain[J]. Lancet, 2011, 377(9784):2215-2225. doi: 10.1016/S0140-6736(11)60245-6 [2] Di Vito C, Mikulak J, Zaghi E, et al. NK cells to cure cancer[J]. Semin Immunol, 2019, 41:101272. doi: 10.1016/j.smim.2019.03.004 [3] Zamarron BF, Chen W. Dual roles of immune cells and their factors in cancer development and progression[J]. Int J Biol Sci, 2011, 7(5):651-658. doi: 10.7150/ijbs.7.651 [4] Inada T, Kubo K, Shingu K. Possible link between cyclooxygenase-inhibiting and antitumor properties of propofol[J]. J Anesth, 2011, 25(4):569-575. doi: 10.1007/s00540-011-1163-y [5] Wall T, Sherwin A, Ma D, et al. Influence of perioperative anaesthetic and analgesic interventions on oncological outcomes:a narrative review[J]. Br J Anaesth, 2019, 123(2):135-150. doi: 10.1016/j.bja.2019.04.062 [6] Missair A, Cata JP, Votta-Velis G, et al. Impact of perioperative pain management on cancer recurrence:an ASRA/ESRA special article[J]. Reg Anesth Pain Med, 2019, 44(1):13-28. doi: 10.1136/rapm-2018-000001 [7] Thomas DA, Boominathan P, Goswami J, et al. Perioperative management of patients with addiction to opioid and non-opioid medications[J]. Curr Pain Headache Rep, 2018, 22(7):52. doi: 10.1007/s11916-018-0704-6 [8] Srikandarajah S, Gilron I. Systematic review of movement-evoked pain versus pain at rest in postsurgical clinical trials and meta-analyses:a fundamental distinction requiring standardized measurement[J]. Pain, 2011, 152(8):1734-1739. doi: 10.1016/j.pain.2011.02.008 [9] Li J, Pourrahmat MM, Vasilyeva E, et al. Efficacy and safety of patientcontrolled analgesia compared with epidural analgesia after open hepatic resection:a systematic review and meta-analysis[J]. Ann Surg, 2019, 270(2):200-208. doi: 10.1097/SLA.0000000000003274 [10] Huepenbecker SP, Cusworth SE, Kuroki LM, et al. Continuous epidural infusion in gynecologic oncology patients undergoing exploratory laparotomy:The new standard for decreased postoperative pain and opioid use[J]. Gynecol Oncol, 2019, 153(2):356-361. https://www.sciencedirect.com/science/article/pii/S0090825819301271 [11] Cummings KC Ⅲ, Zimmerman NM, Maheshwari K, et al. Epidural compared with non-epidural analgesia and cardiopulmonary complications after colectomy:A retrospective cohort study of 20, 880 patients using a national quality database[J]. J Clin Anesth, 2018, 47:12-18. doi: 10.1016/j.jclinane.2018.03.005 [12] Lorimier G, Seegers V, Coudert M, et al. Prolonged perioperative thoracic epidural analgesia may improve survival after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for colorectal peritoneal metastases:A comparative study[J]. Eur J Surg Oncol, 2018, 44(11):1824-1831. doi: 10.1016/j.ejso.2018.08.012 [13] O'Scanaill P, Keane S, Wall V, et al. Single-shot pectoral plane (PECs I and PECs II) blocks versus continuous local anaesthetic infusion analgesia or both after non-ambulatory breast-cancer surgery:a prospective, randomised, double-blind trial[J]. Br J Anaesth, 2018, 120(4):846-853. doi: 10.1016/j.bja.2017.11.112 [14] Choi JJ, Jo YY, Kim SH, et al. Remifentanil-sparing effect of pectoral nerve block typeⅡ in breast surgery under surgical pleth index-guided analgesia during total intravenous anesthesia[J]. J Clin Med, 2019, 8(8):1181. doi: 10.3390/jcm8081181 [15] Fujii T, Shibata Y, Akane A, et al. A randomised controlled trial of pectoral nerve-2(PECS 2) block vs. serratus plane block for chronic pain after mastectomy[J]. Anaesthesia, 2019, 74(12):1558-1562. doi: 10.1111/anae.14856 [16] Mazzinari G, Rovira L, Casasempere A, et al. Interfascial block at the serratus muscle plane versus conventional analgesia in breast surgery:a randomized controlled trial[J]. Reg Anesth Pain Med, 2019, 44(1):52-58. doi: 10.1136/rapm-2018-000004 [17] Tran DQ, Bravo D, Leurcharusmee P, et al. Transversus abdominis plane block:a narrative review[J]. Anesthesiology, 2019, 131(5):1166-1190. doi: 10.1097/ALN.0000000000002842 [18] Zaghiyan KN, Mendelson BJ, Eng MR, et al. Randomized clinical trial comparing laparoscopic versus ultrasound-guided transversus abdominis plane block in minimally invasive colorectal surgery[J]. Dis Colon Rectum, 2019, 62(2):203-210. doi: 10.1097/DCR.0000000000001292 [19] Xu YJ, Sun X, Jiang H, et al. Randomized clinical trial of continuous transversus abdominis plane block, epidural or patient-controlled analgesia for patients undergoing laparoscopic colorectal cancer surgery[J]. Br J Surg, 2020, 107(2):e133-e141. doi: 10.1002/bjs.11403 [20] Sessler DI, Pei L, Huang Y, et al. Recurrence of breast cancer after regional or general anaesthesia:a randomised controlled trial[J]. Lancet, 2019, 394(10211):1807-1815. doi: 10.1016/S0140-6736(19)32313-X [21] Chiu C, Aleshi P, Esserman LJ, et al. Improved analgesia and reduced post-operative nausea and vomiting after implementation of an enhanced recovery after surgery (ERAS) pathway for total mastectomy[J]. BMC Anesthesiol, 2018, 18(1):41. doi: 10.1186/s12871-018-0505-9 [22] Taketa Y, Irisawa Y, Fujitani T. Programmed intermittent bolus infusion versus continuous infusion of 0.2% levobupivacaine after ultrasoundguided thoracic paravertebral block for video-assisted thoracoscopic surgery:A randomised controlled trial[J]. Eur J Anaesthesiol, 2019, 36(4):272-278. doi: 10.1097/EJA.0000000000000945 [23] Zheng X, Feng X, Cai XJ. Effectiveness and safety of continuous wound infiltration for postoperative pain management after open gastrectomy[J]. World J Gastroenterol, 2016, 22:1902-1910. doi: 10.3748/wjg.v22.i5.1902 [24] Nguyen J, Luk K, Vang D, et al. Morphine stimulates cancer progression and mast cell activation and impairs survival in transgenic mice with breast cancer[J]. Br J Anaesth, 2014, 113(Suppl 1):i4-i3. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=HighWire000006330272 [25] Boland JW, McWilliams K, Ahmedzai SH, et al. Effects of opioids on immunologic parameters that are relevant to anti-tumour immune potential in patients with cancer:a systematic literature review[J]. Br J Cancer, 2014, 111(5):866-873. doi: 10.1038/bjc.2014.384 [26] Christian J, Harald I, Teijo S, et al. Patient-controlled analgesia with target-controlled infusion of hydromorphone in postoperative pain therapy[J].Anesthesiology, 2016, 124(1):56-58. doi: 10.1097/ALN.0000000000000937 [27] Maund E, McDaid C, Rice S, et al. Paracetamol and selective and nonselective non-steroidal anti-inflammatory drugs (NSAIDs) for the reduction of morphine-related side effects after major surgery:a systematic review[J]. Br J Anaesth, 2011, 106(3):292-297. doi: 10.1093/bja/aeq406 [28] Namour F, Galien R, Van Kaem T, et al. Safety, pharmacokinetics and pharmacodynamics of GLPG0974, a potent and selective FFA2 antagonist, in healthy male subjects[J]. Br J Clin Pharmacol, 2016, 82(1):139-148. doi: 10.1111/bcp.12900 [29] Sorski L, Melamed R, Matzner P, et al. Reducing liver metastases of colon cancer in the context of extensive and minor surgeries through β-adrenoceptors blockade and COX2 inhibition[J]. Brain Behav Immun, 2016, 58:91-98. doi: 10.1016/j.bbi.2016.05.017 [30] Haldar R, Shaashua L, Lavon H, et al. Perioperative inhibition of betaadrenergic and COX2 signaling in a clinical trial in breast cancer patients improves tumor Ki-67 expression, serum cytokine levels, and PBMCs transcriptome[J].Brain Behav Immun, 2018, 73:294-309. doi: 10.1016/j.bbi.2018.05.014 [31] Freeman J, Crowley PD, Foley AG, et al. Effect of perioperative lidocaine, propofol and steroids on pulmonary metastasis in a murine model of breast cancer surgery[J]. Cancers (Basel), 2019, (5):613. https://www.ncbi.nlm.nih.gov/pubmed/31052479 [32] Dewinter G, Coppens S, Van de Velde M, et al. Quadratus lumborum block versus perioperative intravenous lidocaine for postoperative pain control in patients undergoing laparoscopic colorectal surgery:a prospective, randomized, double-blind controlled clinical trial[J]. Ann Surg, 2018, 268:769-775. doi: 10.1097/SLA.0000000000002888 [33] McNicol ED, Schumann R, Haroutounian S. A systematic review and meta-analysis of ketamine for the prevention of persistent postsurgical pain[J]. Acta Anaesthesiol Scand, 2014, 58(10):1199-1213. doi: 10.1111/aas.12377 [34] 吴新民, 薛张纲, 马虹, 等.右美托咪定临床应用专家共识(2018)[J].临床麻醉学杂志, 2018, 34(8):820-823. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=lcmzxzz201808025 [35] Jessen Lundorf L, KorveniusNedergaard H, Møller AM. Perioperative dexmedetomidine for acute pain after abdominal surgery in adults[J]. Cochrane Database Syst Rev, 2016, 2:CD010358. https://www.ncbi.nlm.nih.gov/pubmed/26889627 [36] Hole J, Hirsch M, Ball E, et al. Music as an aid for postoperative recovery in adults:a systematic review and meta-analysis[J]. Lancet, 2015, 386(10004):1659-1671. doi: 10.1016/S0140-6736(15)60169-6 -




 下载:
下载: