Analysis of relative factors associated with lymph node metastasis in 1 085 patients with invasive lung adenocarcinoma and construction of a nomogram
-
摘要:
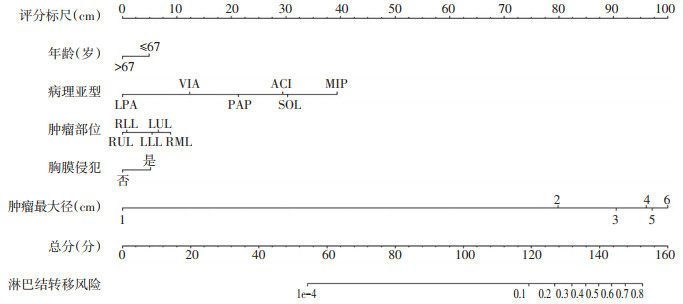
目的 探究浸润性肺腺癌淋巴结转移与肺腺癌病理亚型等相关因素之间的关系。 方法 收集1 085例浸润性肺腺癌患者的相关临床病理资料,对其淋巴结转移情况与年龄、性别、病理亚型、肿瘤部位、肿瘤最大径、胸膜侵犯6项因素之间的关系进行分析。将单因素分析中有意义的变量纳入多因素Logistic回归模型中,以此为基础构建诺模图,并用一致性指数(C-index)、校正模型、受试者工作特征(ROC)曲线等对该模型进行评价。 结果 多因素非条件Logistic回归分析结果显示,年龄≤67岁(OR=1.599,P= 0.036)、病理亚型(OR=1.337,P < 0.001)、肿瘤部位(OR=1.162,P=0.027)、肿瘤最大径(OR=1.765,P < 0.001)、胸膜侵犯(OR=2.179,P < 0.001)为肺癌淋巴结转移的独立风险因素。应用上述因素构建诺模图,对该诺模图模型进行验证,C-index为0.860(95%CI:0.834~0.885),校正曲线有较好的一致性,ROC曲线下面积(AUC)为0.829(95%CI:0.799~0.858)。 结论 年龄≤67岁、病理亚型、肿瘤部位、肿瘤最大径及胸膜侵犯为肺腺癌淋巴结转移的风险因素,对淋巴结转移具有重要预测意义。本研究构建的诺模图预测模型预测能力较好。 -
关键词:
- 浸润性肺腺癌 /
- 淋巴结转移 /
- 病理亚型 /
- 诺模图 /
- 免试者工作特征曲线分析
Abstract:Objective To investigate the relationship between lymph node metastasis of lung adenocarcinoma and relative factors. Methods A total of 1 085 patients diagnosed with invasive lung adenocarcinoma were enrolled. The relationship between lymph node metastasis and relative factors, including age, sex, adenocarcinoma subtype, tumor location, tumor size and pleural invasion, was analyzed statistically. The relative factors were selected using a chi-square test for univariate analysis. Statistically significant prognostic factors were analyzed using a Logistic regression model. Based on this model, a nomogram was developed and evaluated using Harrell's concordance index (Cindex), calibration plots and a receiver operating characteristic curve (ROC). Results The results of multivariate unconditional Logistic regression analysis showed that age ≤67 years (OR=1.599, P=0.036), adenocarcinoma subtype (OR=1.337, P < 0.001), tumor location (OR= 1.162, P=0.027), tumor size (OR=1.765, P < 0.001) and pleural invasion (OR=2.179, P < 0.001) were independent risk factors for lymph node metastasis of lung adenocarcinoma. These factors were incorporated to construct a nomogram. Its C-index was 0.860 (95%CI: 0.834-0.885). The calibration curve showed excellent agreement between the predicted and observed risks of lymph node metastasis of lung adenocarcinoma. The area under the curve (AUC) of the ROC curve was 0.829 (95%CI: 0.799-0.858). Conclusions Age, adenocarcinoma subtype, tumor location, tumor size and pleural invasion were independent risk factors, significant for predicting lymph node metastasis of lung adenocarcinoma. A nomogram was constructed and validated to have a good predictive ability. -
表 1 肺浸润性腺癌相关因素与淋巴转移之间的关系
n(%) 
表 2 非条件多因素Logistic回归分析

-
[1] Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019[J]. CA Cancer J Clin, 2019, 69(1): 7-34. doi: 10.3322/caac.21551 [2] 郑荣寿, 孙可欣, 张思维, 等. 2015年中国恶性肿瘤流行情况分析[J]. 中华肿瘤杂志, 2019, 41(1): 19-28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005 [3] Park JK, Kim JJ, Moon SW, et al. Lymph node involvement according to lung adenocarcinoma subtypes: lymph node involvement is influenced by lung adenocarcinoma subtypes[J]. J Thorac Dis, 2017, 9 (10): 3903-3910. doi: 10.21037/jtd.2017.08.132 [4] Chen C, Chen Z, Cao H, et al. A retrospective clinicopathological study of lung adenocarcinoma: Total tumor size can predict subtypes and lymph node involvement[J]. Clin Imaging, 2018, 47: 52-56. doi: 10.1016/j.clinimag.2017.08.009 [5] Zhao X, Zhang Y, Qian K, et al. Prognostic significance of the international association for the study of lung cancer/american thoracic society/european respiratory society classification of stage Ⅰlung adenocarcinoma: A retrospective study based on analysis of 110 Chinese patients[J]. Thorac Cancer, 2017, 8(6): 565-571. doi: 10.1111/1759-7714.12464 [6] Motono N, Matsui T, Machida Y, et al. Prognostic significance of histologic subtype in pStageⅠlung adenocarcinoma[J]. Med Oncol, 2017, 34(6): 100. doi: 10.1007/s12032-017-0962-x [7] 田璇, 孙蕾娜, 王静, 等. 最新国际肺腺癌分类方法回顾性分析具有细支气管肺泡癌特征的肺腺癌209例[J]. 中国肿瘤临床, 2013, 40(8): 475- 478. doi: 10.3969/j.issn.1000-8179.2013.08.011 [8] Fukutomi T, Hayashi Y, Emoto K, et al. Low papillary structure in lepidic growth component of lung adenocarcinoma: a unique histologic hallmark of aggressive behavior[J]. Hum Pathol, 2013, 44(9): 1849- 1858. doi: 10.1016/j.humpath.2013.02.008 [9] Eguchi T, Kadota K, Park B J, et al. The new IASLC-ATS-ERS lung adenocarcinoma classification: what the surgeon should know[J]. Semin Thorac Cardiovasc Surg, 2014, 26(3): 210-222. doi: 10.1053/j.semtcvs.2014.09.002 [10] Yu Y, Jian H, Shen L, et al. Lymph node involvement influenced by lung adenocarcinoma subtypes in tumor size ≤3 cm disease: A study of 2268 cases[J]. Eur J Surg Oncol, 2016, 42(11): 1714-1719. doi: 10.1016/j.ejso.2016.02.247 [11] Kuroda H, Sakao Y, Mun M, et al. Lymph node metastases and prognosis in left upper division non-small cell lung cancers: the impact of in terlobar lymph node Metastasis[J]. PLoS One, 2015, 10(8): e0134674. doi: 10.1371/journal.pone.0134674 [12] Ye W F, Xie X, Yang H, et al. Resectable left lower lobe non-small cell lung cancer with lymph node metastasis is related to unfavorable outcomes[J]. Chin J Cancer, 2016, 35: 7. doi: 10.1186/s40880-015-0069-8 [13] 徐秋萍, 何斐, 刘志强, 等. 性别对非小细胞肺癌预后的影响分析[J]. 中华流行病学杂志, 2017, 38(2): 244-247. doi: 10.3760/cma.j.issn.0254-6450.2017.02.022 [14] Chen K, Yang F, Jiang G, et al. Development and validation of a clinical prediction model for N2 lymph node metastasis in non-small cell lung cancer[J]. Ann Thorac Surg, 2013, 96(5): 1761-1768. doi: 10.1016/j.athoracsur.2013.06.038 [15] O'connell OJ, Almeida FA, Simoff MJ, et al. A Prediction model to help with the assessment of adenopathy in lung cancer: HAL[J]. Am J Respir Crit Care Med, 2017, 195(12): 1651-1660. doi: 10.1164/rccm.201607-1397OC [16] Xia W, Wang A, Jin M, et al. Young age increases risk for lymph node positivity but decreases risk for non-small cell lung cancer death[J]. Cancer Manag Res, 2018, 10: 41-48. doi: 10.2147/CMAR.S152017 [17] Chen T, Luo J, Wang R, et al. Visceral pleural invasion predict a poor survival among lung adenocarcinoma patients with tumor size ≤ 3 cm [J]. Oncotarget, 2017, 8(39): 66576-66583. doi: 10.18632/oncotarget.16476 [18] Kang JH, Kim KD, Chung KY. Prognostic value of visceral pleura invasion in non-small cell lung cancer[J]. Eur J Cardiothorac Surg, 2003, 23(6): 865-869. doi: 10.1016/S1010-7940(03)00119-2 [19] Shimizu K, Yoshida J, Nagai K, et al. Visceral pleural invasion is an invasive and aggressive indicator of non- small cell lung cancer[J]. J Thorac Cardiovasc Surg, 2005, 130(1): 160-165. doi: 10.1016/j.jtcvs.2004.11.021 [20] Kudo Y, Saji H, Shimada Y, et al. Impact of visceral pleural invasion on the survival of patients with non-small cell lung cancer[J]. Lung Cancer, 2012, 78(2): 153-160. doi: 10.1016/j.lungcan.2012.08.004 -




 下载:
下载: