Clinicopathological characteristics of seven cases of atypical neurofibromatous neoplasm of uncertain biologic potential
-
摘要:
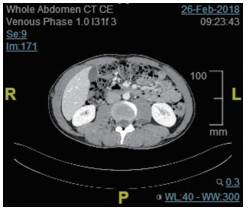
目的 探讨生物潜能未定非典型神经纤维瘤(atypical neurofibromatous neoplasm of uncertain biologic potential,ANNUBP)的临床病理特征、免疫表型、分子遗传学改变。 方法 分析2014年12月至2020年8月收集于北京大学国际医院病理诊断为非典型或富于细胞性神经纤维瘤14例患者的临床资料,其中7例具有ANNUBP的特征,光镜观察肿瘤细胞形态、免疫表型特征、并进行总结。 结果 ANNUBP中男性5例,女性2例,年龄14~44岁(平均年龄27岁,中位年龄27岁);6例位于腹膜后,1例位于头颈部,最大径4.5~21.5 cm,平均11.0 cm,界限较清。镜下肿瘤细胞可见细胞异型性、丰富密集、失去神经纤维瘤结构和/或核分裂像增加(>1/50 HPF和<3/10 HPF);其中4例多次复发,2例进展为恶性外周神经鞘膜瘤(malignant peripheral nerve sheath tumor,MPNST),1例无瘤生存,复发率85.71%(6/7),恶变率28.57%(2/7);S-100、SOX-10、H3K27Me3在7例中均弥漫强表达,1例CD34染色显示网状结构消失,Ki-67增殖指数<2%~5%。 结论 ANNUBP是具有较高复发率和恶变率的肿瘤,术后应结予相应的辅助治疗,并密切随访,同时也应避免过度治疗;结合免疫组织化学,有助于其诊断和鉴别诊断。 -
关键词:
- 生物潜能未定非典型神经纤维瘤 /
- 复发 /
- 恶性外周神经鞘膜瘤
Abstract:Objective To investigate the clinicopathological characteristics, immunophenotypes, and molecular genetic changes in atypical neurofibromatous neoplasm of uncertain biologic potential (ANNUBP). Methods Fourteen cases of atypical or hypercellularity neurofibroma were collected from surgical specimens at the Pathology Department of Peking University International Hospital from December 2014 to August 2020. Seven cases had characteristics of ANNUBP. Microscopy, immunophenotype analysis, and summary were performed. Results There were five males and two females, with ages ranging 14-44 years (average and median ages were 27 and 27 years, respectively); six had ANNUBP located in the retroperitoneum, whereas one was located in the head and neck. The maximum diameter ranged from 4.5 to 21.5 cm, the mean diameter was 11 cm, and the boundary was clear. Seven cases showed nuclear atypia, hypercellularity, loss of neurofibroma architecture, and increased mitotic image (>1/50 and<3/10 HPF). Four cases recurred multiple times, two patients developed malignant peripheral nerve sheath tumor (MPNST), and one patient survived without tumor. The recurrence rate was 85.71% (6/7) and the malignant transformation rate was 28.57% (2/7). S-100, Sox-10, and H3K27Me3 were all diffused and strongly expressed in seven cases. CD34 showed the disappearance of reticular structure in one case, and the Ki-67 proliferation index was less than 2%-5%. Conclusions ANNUBP is a tumor with high recurrence and malignant transformation rates. Postoperative adjuvant therapy and close follow-up combined with immunohistochemistry should be provided, and overtreatment should be avoided, thus aiding its diagnosis. -
表 1 ANNUBP的临床病理特征

-
[1] Miettinen MM, Antonescu CR, Fletcher CDM, et al. Histopathologic evaluation of atypical neurofibromatous tumors and their transformation into malignant peripheral nerve sheath tumor in patients with neurofibromatosis 1-a consensus overview[J]. Hum Pathol, 2017, 67: 1-10. doi: 10.1016/j.humpath.2017.05.010 [2] Schaefer IM, Fletcher CD. Malignant peripheral nerve sheath tumor (mpnst) arising in diffuse-type neurofibroma clinicopathologic characterization in a series of 9 cases[J]. Am J Surg Pathol, 2015, 39 (9): 1234-1241. doi: 10.1097/PAS.0000000000000447 [3] Miettinen MM, Antonescu CR, Histopathologic evaluation of atypical neurofibrofibromatous tumors and their transformation into malignant peripheral nerve sheath tumor in neurofibromatosis 1 patients-A consensus overview[J]. Hum Pathol, 2017, 67: 1-10. doi: 10.1016/j.humpath.2017.05.010 [4] Zhao F, Zhang S, Du J, et al. Comparison of clinical, histopathological, and genomic features between malignant peripheral nerve sheath tumors and cellular schwannomas of the eighth cranial nerve: a case series[J]. World neurosurg, 2019, 122: e487-e497. doi: 10.1016/j.wneu.2018.10.087 [5] Meyer A, Billings SD. What's new in nerve sheath tumors[J]. Virchows Arch, 2020, 476(1): 65-80. doi: 10.1007/s00428-019-02671-0 [6] Kourea HP, Cordon-Cardo C, Dudas M, et al. Expression of p27(kip) and other cell cycle regulators in malignant peripheral nerve sheath tumors and neurofibromas: the emerging role of p27(kip) in malignant transformation of neurofibromas[J]. Am J Pathol, 1999, 155(6): 1885-1891. doi: 10.1016/S0002-9440(10)65508-3 [7] Karpinsky G, Krawczyk MA, Swieszewska E, et al. Tumor expression of surviving, p53, cyclin D1, osteopontin and fibronectin in predicting the response to neo-adjuvant chemotherapy in children with advanced malignant peripheral nerve sheath tumor[J]. J Cancer Res Clin Oncol, 2018, 144(3): 519-529. doi: 10.1007/s00432-018-2580-1 [8] Tajima S, Koda K, A neurogenic tumor containing a low-grade malignant peripheral nerve sheath tumor (MPNST) component with loss of p16 expression and homozygous deletion of CDKN2A/p16: a case report showing progression from a neurofibroma to a highgrade MPNST[J]. Int J Clin Exp Pathol, 2015, 8(5): 5113-5120. http://www.ncbi.nlm.nih.gov/pubmed/26191206 [9] Kaplan HG, Rostad S, Ross JS, et al. Genomic profiling in patients with malignant peripheral nerve sheath tumors reveals multiple pathways with targetable mutations[J]. J Natl Compr Canc Netw, 2018, 16(8): 967-974. doi: 10.6004/jnccn.2018.7033 [10] Le Guellec S, Macagno N, Velasco V, et al. Loss of H3K27 trimethylation is not suitable for distinguishing malignant peripheral nerve sheath tumor from melanoma: a study of 387 cases including mimicking lesions[J]. Mod Pathol, 2017, 30(12): 1677-1687. doi: 10.1038/modpathol.2017.91 [11] Prieto-Granada CN, Wiesner T, Messina JL, et al. Loss of H3K27me3 expression is a highly sensitive marker for sporadic and radiationinduced MPNST[J]. Am J Surg Pathol, 2016, 40(4): 479-489. doi: 10.1097/PAS.0000000000000564 [12] Gilder HE, Puffer RC, Spinner RJ, et al. Low-Grade malignant peripheral nerve sheath tumor mimicking schwannoma: role and importance of trimethylated H3K27M staining[J]. World Neurosurg, 2018, 117: 178-181. doi: 10.1016/j.wneu.2018.06.035 [13] Otsuka H, Kohashi K, Yoshimoto M, et al. Immunohistochemical evaluation of H3K27 trimethylation in malignant peripheral nerve sheath tumors[J]. Pathol Res Pract, 2018, 214(3): 417-425. doi: 10.1016/j.prp.2017.12.015 [14] Evans HL. Sporadic superficial diffuse neurofibromas withrepeated local recurrence over many years repeated local recurrence over many years and a tendency toward malignant change: a report of 3 cases[J]. Am J Surg Pathol, 2013, 37(7): 987-994. doi: 10.1097/PAS.0b013e31827c96f4 [15] 赵明, 徐明鑫, 王宇彬, 等. 去分化脂肪肉瘤的组织学诊断与鉴别诊断[J]. 中华病理学杂志, 2019, 48(7): 573-579. [16] 化宏金, 吴靓, 孙浩然, 等. 伴有脑膜上皮细胞样旋涡状特征的去分化脂肪肉瘤六例临床病理学观察[J]. 中华病理学杂志, 2020, 49(2): 139-144. doi: 10.3760/cma.j.issn.0529-5807.2020.02.007 [17] Pekmezci M, Cuevas-Ocampo AK, Perry A, et al. Significance of H3K27me3 loss in the diagnosis of malignant peripheral nerve sheath tumors[J]. Mod Pathol, 2017, 30(12): 1710-1719. doi: 10.1038/modpathol.2017.97 [18] Beert E, Brems H, Daniëls B, et al. Atypical neurofibromas in neurofibromatosis type 1 are premalignant tumor[J]. Genes Chromosomes Cancer, 2011, 50(12): 1021-1032. doi: 10.1002/gcc.20921 -




 下载:
下载: